Understanding IgA Nephropathy and the Role of Complement Activation
The recent APPLAUSE-IgAN trial has stirred conversation among clinicians and researchers alike. This trial, which examined the effects of the complement factor B inhibitor iptacopan on IgA nephropathy, has provided fresh insights into the role of the complement system in this kidney disease. In an opinion piece presented in a renowned medical journal, experts discussed how treating IgA nephropathy by reducing proteinuria might be achieved by targeting a specific part of the immune response.
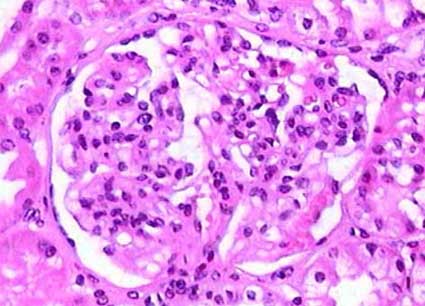
For more than 50 years, it has been known that C3 is deposited in over 90% of IgA nephropathy cases. The trial findings point to complement activation as one of the key drivers behind the condition’s progression. However, as promising as these findings are, they also remind us that managing the disease is layered with tricky parts, tangled issues, and some rather complicated pieces that demand a deeper look.
Exploring the Potential of Iptacopan in Modern Nephrology
Iptacopan works by inhibiting complement factor B, a critical protein in the alternative complement pathway. By reducing the activity of this molecule, the therapy decreases the cascade that typically drives the inflammatory response in the kidney. The reduction in proteinuria observed in the trial signals that iptacopan might offer a new direction for addressing the underlying causes of IgA nephropathy.
The approach of using drug therapy to tackle this facet of the immune system is both innovative and super important. Yet, while many celebrate this advance, others wonder about the broader implications of targeting the alternative complement pathway. Is it enough to merely cut down proteinuria, or are there other hidden complexities in the disease process that continue to persist?
It is also essential to consider the nerve-racking possibility that not all patients will respond the same way to such a treatment. With IgA nephropathy being a condition that carries many little details in its disease mechanism, understanding who benefits most from this therapy is a challenge that clinicians are just starting to tackle.
Analyzing Complement Activation in IgA Nephropathy: A Closer Look at the Fine Points
One of the main takeaways from the trial is that complement activation does not occur uniformly among all patients with IgA nephropathy. Despite the general observation of C3 deposition, the intensity and nature of complement activation can vary considerably. This disparity hints at several biological twists and turns that make it tough to design a one-size-fits-all treatment regimen.
The commentary in the journal editorial stresses that while the trial successfully showed a reduction in proteinuria, the study did not fully account for the heterogeneity in complement activation. In simpler words, while cutting proteinuria serves as a promising biomarker of efficacy, there may be additional factors at play that might affect long-term outcomes in real-world settings.
In our view, the decision to specifically target the alternative complement pathway must therefore be accompanied by careful monitoring. Healthcare professionals should monitor various markers of disease activity beyond proteinuria to ensure that interventions are truly addressing the disease’s small distinctions.
Challenges in Managing Heterogeneous Disease Profiles
One critical aspect of studying and managing IgA nephropathy is understanding the varying levels of complement activation among patients. Here are some of the tricky parts involved:
- Differences in Immune Response: Patients exhibit a broad range of complement activity, meaning that a treatment that works well for one patient might be less effective for another due to these subtle differences.
- Biomarker Limitations: While proteinuria remains a super important marker, it only captures part of the picture. More refined biomarkers are needed to get into the nitty-gritty of disease progression.
- Individual Variation in Kidney Function: The state of kidney health varies widely and can impact how well a patient might respond to inhibition of the complement pathway.
These points underscore the importance of not only adopting innovative therapies like iptacopan but also keeping a close eye on patient-specific responses to treatment. It’s a reminder that while we aim to find your way through these complex pathways, accounting for every little twist is both necessary and challenging.
Examining Clinical Trial Data: Beyond the Surface of Proteinuria Reduction
While the APPLAUSE-IgAN trial clearly demonstrated that iptacopan can lower protein levels in urine, the broader clinical picture remains to be seen. The reduction in proteinuria is undeniably a positive sign. Still, it is essential to explore whether this biochemical improvement will translate into long-term benefits, such as delayed progression to end-stage kidney disease or improved patient survival.
Critical questions arise when we poke around the trial data:
- How sustainable is the reduction in proteinuria over the long haul?
- Can we assess the therapy’s effect on the overall immune environment in the kidneys?
- What are the potential side effects when the complement pathway is inhibited over a prolonged period?
These questions represent more than mere fine shades of inquiry; they are essential to understanding the drug’s role in clinical practice. The trial’s design offers a starting point, but additional studies — particularly longer-term and real-world investigations — are needed to fully explore these areas. By mapping out the long journey from controlled trial settings to everyday clinical practice, researchers and clinicians alike must figure a path that accommodates these varied trajectories.
Potential Implications for Patient Care
Assuming that longer trials confirm the benefits observed so far, the implications for patient care could be significant:
- A Shift in Treatment Paradigms: If complement inhibition proves effective over many years, it could lead to a new standard of care for managing IgA nephropathy.
- Personalized Medicine Approaches: Recognizing that patients show different levels of complement activation might pave the way to customized treatment plans based on an individual’s immune profile.
- Reduced Progression to Severe Disease: By targeting the early mechanisms of kidney damage, early intervention with drugs like iptacopan could reduce the risk of progressing to more severe, irreversible kidney damage.
This strategy would not only help preserve kidney function but also improve quality of life by mitigating some of the nerve-racking complications that frequently accompany advanced kidney disease.
Addressing the Tricky Parts: Heterogeneity and Patient Selection
It is critical to remember that IgA nephropathy is not a uniform condition. Even though the majority of patients share the common sign of C3 deposition, the intensity and the timing of complement activation can differ. This means that while iptacopan may be a promising therapy, it might not be the ideal solution for everyone.
Sorting out which patient will benefit the most poses its own set of challenges. Here are some key factors that must be taken into consideration:
| Factor | Consideration |
|---|---|
| Baseline Disease Severity | Patients with advanced disease might react differently compared to those in earlier stages. |
| Degree of Complement Activation | The level of C3 deposition may influence the therapeutic response to iptacopan. |
| Genetic Markers | Potential genetic predispositions that affect immune response should be evaluated. |
| Concurrent Treatments | Co-administration with other immune-modulating drugs could alter outcomes. |
This table underscores the delicate balance required when choosing patients for complement inhibition therapy. Each category represents a complicated piece of a larger puzzle that clinicians must assemble in order to figure a path toward more personalized treatment approaches.
Weighing the Benefits Against Possible Risks and Side Effects
Every new therapy brings with it its set of potential risks alongside the benefits. While reducing proteinuria is an essential marker of efficacy, targeting a central part of the immune system might open the door to unintended consequences. The alternative complement pathway plays roles in protecting the body from infections and other immune challenges, so dampening its activity can have broader implications.
Here is a bullet list summarizing the potential pros and cons of using iptacopan:
- Pros:
- Clear reduction in proteinuria, which may indicate a slowdown in kidney damage.
- Potential to delay the progression to more severe kidney failure.
- Support for the theory that complement activation is a key element in IgA nephropathy.
- Cons:
- Risk of infections due to dampened immune response.
- Unclear long-term safety profile in a real-world setting.
- Variability in patient responses, which complicates treatment protocols.
The list above helps us to see the balance that must be maintained between therapeutic advantages and the nerve-racking potential for adverse effects. It is crucial for clinicians to work through these challenges by carefully monitoring patients over time and being prepared to adjust treatment strategies as needed.
Diving Into the Clinical Implications: A Broader Perspective
While the APPLAUSE-IgAN trial represents an exciting advance in our understanding of IgA nephropathy, it is vital to look at the broader context. Clinical research does more than just spot a single promising signal—it serves as a stepping stone toward a more comprehensive approach to disease management.
The trial results stimulate several discussions on key topics:
- The Evolution of Targeted Therapies: Iptacopan’s success in reducing proteinuria highlights a wider trend in medicine toward targeting specific pathways. This approach, focusing on the hidden complexities of immune system dysregulation, can be applied to many other conditions.
- Real-World Application: While controlled trial environments are essential for evaluating drug efficacy, the transition to everyday clinical settings often brings new challenges. There remain many small distinctions between trial populations and the broader, more diverse patient communities seen in routine practice.
- Economic and Accessibility Considerations: New therapies, especially those that come from high-tech innovations in medicine, are often expensive. Ensuring that such advances are accessible to all who might benefit is on edge with public health priorities.
It is equally critical that researchers consider patient perspectives when translating these findings into real-world practice. Patients often face overwhelming and intimidating treatment decisions, and clear communication about both benefits and potential risks can alleviate some of those concerns.
Integrating Alternative Approaches in Managing IgA Nephropathy
Modern medicine continues to explore ways to integrate alternative approaches with conventional therapies in managing complex diseases like IgA nephropathy. The insights from complement inhibition research have inspired clinicians to think beyond traditional strategies.
Some alternative treatment approaches being considered include:
- Nutritional Interventions: Diet modifications that reduce inflammation and support kidney health are gaining attention. Foods rich in antioxidants and omega-3 fatty acids may help ease the inflammatory state often seen in kidney diseases.
- Mind-Body Practices: Techniques such as yoga, meditation, and mindfulness can play a supportive role by reducing stress—a factor that might indirectly influence immune function and inflammation.
- Herbal and Supplement-Based Therapies: There is emerging interest in certain herbal medicines that have anti-inflammatory properties. However, it is essential to balance such treatments with evidence-based therapies and maintain close oversight by healthcare professionals.
While none of these alternative approaches replace the need for targeted pharmacologic therapy, their potential to complement the main treatment plan offers a more rounded approach. Such multimodal treatment strategies demand that healthcare providers take a closer look at every small twist in the patient’s overall health picture, ensuring that care is as comprehensive and individualized as possible.
Challenges in Clinical Practice: Finding Your Way Through Uncertainty
The application of innovative therapies like iptacopan in a clinical setting is full of challenging parts and confusing bits. Physicians must make their way through treatment decisions that are loaded with issues—ranging from patient selection to long-term monitoring and potential side effects. The environment in which these decisions are made is far from static, incorporating rapidly changing evidence and real-world experiences.
In everyday practice, the following considerations become key to managing these twists and turns:
- Continuous Education: Healthcare professionals must commit to ongoing education in the latest developments. Regular updates through medical journals, conferences, and online platforms can provide vital insights into how novel therapies perform outside the controlled conditions of clinical trials.
- Shared Decision-Making: Patients should be active participants in their treatment plans. Explaining both the promise and the potential pitfalls of therapies creates a partnership between clinicians and their patients, ensuring that treatment decisions are aligned with patient values and preferences.
- Multidisciplinary Collaboration: Complex cases benefit from input by a team of experts, including nephrologists, immunologists, dietitians, and mental health professionals. This team-based approach can help balance the various factors at play and offer more holistic care.
By embracing these strategies, clinicians can better find their way through the nerve-racking and intimidating challenges that come with managing a disease as multi-faceted as IgA nephropathy. Maintaining flexibility and a commitment to the latest evidence is key to optimizing patient outcomes.
Looking Ahead: The Future of Complement Inhibition
The future of treatment for IgA nephropathy looks promising, but it is also riddled with tension about how best to implement these therapies. The success of iptacopan in clinical trials has set the stage for a new wave of research that may further unravel the subtle details of complement activation and its role in kidney injury.
Future research directions might include:
- Long-Term Outcome Studies: As we mentioned earlier, it is super important to track patients over a longer term to truly understand the benefits and any possible hidden issues associated with complement inhibition.
- Comparative Effectiveness Research: Comparing iptacopan with other emerging therapies can help identify the best treatment protocols while also illuminating small distinctions that might otherwise be overlooked.
- Biomarker Discovery: Developing and validating new biomarkers that can more accurately gauge complement activity will provide clinicians with better tools for monitoring disease progression and treatment response.
- Expanding Patient Cohorts: Including more diverse patient populations in future studies will help ensure that findings are applicable to real-world practice, where the patient group is invariably diverse and full of intricacies.
These research initiatives will be super important not only for refining existing therapies but also for opening up new avenues to treat and possibly prevent the progression of IgA nephropathy. As we learn more about the hidden complexities of the alternative complement pathway, our ability to tailor treatments to individual patient needs will only grow.
Conclusion: A Balanced Approach to Advancing Kidney Care
The conversation sparked by the APPLAUSE-IgAN trial underscores the promise and the challenges of using complement inhibition to treat IgA nephropathy. Iptacopan’s ability to reduce proteinuria represents an important step forward, yet the journey to fully understanding and managing the disease is still very much underway.
This editorial has attempted to shine a light on both the bright prospects emerging from this research and the many nerve-racking, intimidating obstacles that remain. The message is clear: while targeting the alternative complement pathway is a super important strategy, it comes with its fair share of tricky parts, tangled issues, and subtle details that require ongoing attention.
For clinicians on the front lines, the future involves not only embracing new treatments but also continuously learning, adapting, and collaborating with a multidisciplinary team. It means weighing the benefits of reduced proteinuria against the potential risks, while also integrating supportive approaches ranging from dietary interventions to mind-body practices.
Patients, for their part, stand to gain from a more personalized approach that considers their unique profile, the degree of complement activation, and their overall health status. In this rapidly evolving field, open and frequent communication between patients and their healthcare providers is key to successfully working through the uncertainties of advanced kidney care.
In conclusion, while current research offers a promising glimpse into the future of IgA nephropathy treatment, many layers of complexity still need to be tackled. With continued research, careful patient selection, and a willingness to explore both conventional and alternative approaches, the path forward looks promising. The journey involves figuring a clear path through the nerve-racking twists and turns of immune system modulation, but the potential rewards for patient outcomes make every step worth the effort.
As we continue to navigate the challenging landscape of kidney disease, it is our collective responsibility as healthcare providers, researchers, and patient advocates to ensure that every new discovery translates into tangible improvements in care. The balance between innovation and cautious, individualized care will define the trajectory of IgA nephropathy management in the years to come.
Originally Post From https://www.nejm.org/doi/abs/10.1056/NEJMc2503117
Read more about this topic at
Therapeutic targeting of the complement system – PMC
Therapeutic Targeting of the Complement System