Exploring Non-Invasive Treatments in Skin Cancer Care
The field of cutaneous oncology has seen remarkable advancements over the years. More than ever before, dermatologists are stepping away from solely surgical interventions to embrace methods that treat skin cancers in less invasive ways. In our practice, managing the tricky parts of skin conditions such as actinic keratoses (AKs) and non-melanoma skin cancers (NMSC) requires that clinicians find your way through a maze of treatment options that are both effective and cosmetically considerate. This approach is especially key when treating sensitive areas like the face, where minimizing scarring is super important.
At the heart of these emerging trends is a focus on patient-centered care that balances clinical efficacy with quality-of-life considerations. As medical professionals and patients alike dive in to understand the benefits and limitations of non-surgical therapies, it is essential to appreciate the small distinctions that make these options noteworthy. This op-ed intends to explore the current landscape of non-invasive treatments, highlighting practical case studies and expert opinions that guide our decision-making in everyday clinical practice.
Case Studies: Fine Points in Managing Actinic Keratoses and Non-Melanoma Skin Cancer
One of the most striking examples of non-invasive treatment is the optimized management of actinic keratoses, a condition that many practitioners face on a daily basis. Through practical case studies, experts illustrate how tailoring treatment protocols may help overcome the tangled issues that often accompany skin cancers.
During recent expert meetings, clinicians shared detailed accounts of how they manage AK cases using various field therapies. For instance, the use of tirbanibulin and a combination of 5-fluorouracil (5-FU) with topical calcipotriene has shown promising results. These approaches not only shorten the treatment duration but also help reduce the risk of recurrence. In these cases, the dose adjustments and timing of applications were carefully planned to avoid further complications such as scarring or unwanted skin changes.
Key Approaches in Daily Practice
- Field Therapies: Optimizing the timing and dosage of applications using agents like tirbanibulin and 5-FU combinations.
- Case-Based Evaluations: Using real-life examples to demonstrate the effectiveness of personalized treatments.
- Cosmetic Considerations: Prioritizing non-scarring methods when treating areas on the face or other sensitive locations.
This kind of methodical approach is not without its challenges. The confusing bits and twists and turns encountered during treatment planning demand that clinicians dig into the data and get into discussions on best practices. Through comprehensive evaluations and follow-ups, practitioners can fine-tune a treatment protocol that respects both the integrity of the skin and the overall health of the patient.
Innovative Photodynamic Therapy: Minimizing Pain and Enhancing Efficacy
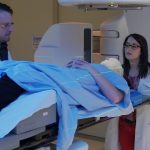
Photodynamic therapy (PDT) stands out as a powerful non-surgical intervention, particularly due to evolving strategies that focus on improving patient comfort and treatment outcomes. Not long ago, PDT was often seen as a last resort characterized by its intimidating side effects, particularly pain during treatment. However, with innovative approaches now available, clinicians have found ways to manage these nerve-racking aspects and even enhance the overall efficacy of the procedure.
Recent discussions during conferences revealed advances in pain mitigation techniques with PDT. The focus has shifted toward ensuring that patients experience minimal discomfort while still achieving excellent clinical results. It is now clear that optimizing these techniques is a matter of paying attention to the little details—such as the wavelength of the light used, the concentration of the photosensitizing agents, and the duration of exposure. By adjusting these subtle parts, practitioners can significantly enhance patient comfort and treatment efficacy.
For many patients, the potential benefits of PDT outweigh any temporary discomfort, especially when it comes to reducing the need for more invasive procedures. When used as part of a broader treatment strategy, PDT can help limit the visible evidence of treatment on sensitive skin areas while successfully managing superficial skin cancers.
Advantages of the Updated Photodynamic Approach
- Improved Patient Comfort: New methods focus on reducing the pain associated with light therapy sessions.
- Efficacy Enhancements: Better outcomes are achieved through optimized dosing and improved light delivery systems.
- Cosmetic Benefits: Non-scarring techniques are particularly beneficial for lesions located on the face or other delicate areas.
These advancements are a testament to the progress in non-surgical treatments and represent a shift in the way dermatologists manage cutaneous oncology. With a commitment to refining the intricate details of PDT protocols, the pathway forward looks promising for patients who have been weighed down by the nerve-racking prospect of invasive procedures.
Emerging Data on 10% Aminolevulinic Acid Gel for Superficial Basal Cell Carcinoma
One of the most promising developments in non-invasive treatment options is the potential FDA approval of 10% aminolevulinic acid gel, a therapy that has produced encouraging phase 3 data. This treatment is geared toward managing superficial basal cell carcinoma (BCC), a type of skin cancer that, while common, requires treatments that minimize disruption to a patient’s appearance—especially when located on socially sensitive areas like the face.
The latest clinical trials have demonstrated that this gel-based therapy can achieve high efficacy, reducing the tumor burden with minimal side effects. The appeal lies in its ability to be applied directly to the lesion, allowing for a localized treatment that circumvents the need for excisional surgery. For many patients, the idea of applying a gel rather than undergoing surgery is not only more appealing but also less disruptive to their lives. As practitioners figure a path through treatment options, data from these studies are increasingly influential in changing treatment protocols.
The potential benefits are underscored by the fact that this innovative gel provides a non-invasive alternative that maintains excellent cosmetic outcomes. With FDA approval anticipated in the near future, clinicians are excited about the prospect of incorporating this therapy into standard practice, as it fills a crucial gap in the treatment arsenal against superficial BCC.
Highlights of the 10% Aminolevulinic Acid Gel Data
- Efficacy Results: Phase 3 data show high success rates in reducing lesion sizes and preventing recurrence.
- Cosmetic Outcomes: The gel minimizes scarring, which is a super important consideration for treatments on the face.
- User-Friendly Application: The direct application process simplifies treatment protocols and enhances patient compliance.
These highlighted points provide a clear picture of why this non-surgical option is gaining attention in clinical circles. As the larger dermatologic community reviews these insights, the anticipation is that this new treatment will soon become a cornerstone of managing superficial BCC in non-invasive ways.
Learning from Real-World Scenarios: Practical Wisdom in Managing Skin Cancers
One of the best ways to understand the effectiveness of non-surgical approaches in cutaneous oncology is by looking at real-world examples. The use of clinical case studies in educational meetings, such as those from the Maui Derm NP+PA Fall, offers a window into the small distinctions that can influence treatment outcomes. Through these sessions, seasoned practitioners have shared experiences that help others figure a path through complicated pieces of decision-making.
For many clinicians, the challenge lies in steering through the nerve-racking aspects of daily practice. Actinic keratoses are just one example: a condition that appears frequently demands that doctors get into the nitty-gritty of treatment adjustments. By analyzing patient histories, treatment responses, and follow-up results, practitioners can learn from each case. This collaborative method not only improves individual patient care but also contributes to a broader understanding of skin cancer management.
Participating in these discussions allows practitioners to dissect complicated treatment algorithms, balancing efficacy with cosmetic outcomes. They often share tips on mixing and matching pharmacological agents, like combining 5-FU with calcipotriene, to achieve a faster and safer resolution of lesions. Such insights are invaluable because they result from trial, error, and careful observation—helping to guide therapy in real-life rather than just in theory.
Benefits of a Case-Based, Collaborative Approach
- Peer-to-Peer Learning: Clinicians share their experiences, discussing both successes and the scary setbacks encountered in treatment.
- Comprehensive Evaluations: By assessing the fine shades of treatment responses, strategies can be adjusted to improve future outcomes.
- Enhanced Decision-Making: Learning from diverse clinical experiences empowers professionals to make informed, case-tailored treatment decisions.
This collaborative learning environment is key to managing the loaded challenges of skin cancer therapy. It provides a platform for medical professionals to talk about the brave new world of non-surgical treatment options, ensuring that they are better prepared for each patient’s unique circumstances.
Balancing Efficacy and Cosmetic Outcomes in Treatment Plans
When it comes to dealing with skin cancers, one of the most delicate challenges is balancing the need for effective cancer control with the desire to maintain a patient’s appearance. This balance becomes particularly important when managing lesions located on the face, scalp, or other highly visible areas. Patients naturally favor treatments that not only rid them of cancer but also preserve their self-image.
Cosmetic outcomes have, in recent years, taken center stage in treatment planning. Non-surgical approaches, such as PDT and topical therapies, allow clinicians to carefully steer through treatment decisions that take into account both the physical health and psychological well-being of the patient. By paying attention to the little details—such as minimizing scarring and avoiding noticeable pigment changes—practitioners can offer solutions that are as aesthetically pleasing as they are medically effective.
Even when faced with deeper, more extensive lesions, the guiding principle remains: choose therapies that limit disfigurement without compromising on cancer control. This often means embracing innovative approaches that might initially seem off-putting due to their novelty, but once their benefits are revealed, they quickly become preferred options in the clinic.
Strategies to Achieve a Dual Focus on Health and Appearance
- Targeted Therapy Selection: Select treatments that specifically target cancer cells while sparing surrounding healthy tissue.
- Optimizing Treatment Parameters: Adjust doses and treatment durations to minimize adverse effects while ensuring efficacy.
- Patient Communication: Clear dialogue about treatment expectations helps in aligning medical outcomes with cosmetic goals.
These tactical approaches are critical in modern dermatologic care. The ability to thoughtfully combine efficacy and cosmetic considerations is what ultimately elevates the patient experience and drives the evolution of treatment protocols.
Integrating a Multidisciplinary Approach in Cutaneous Oncology
The evolution of non-surgical treatments in dermatology underscores the importance of a multidisciplinary approach. By teaming up with specialists from various fields—ranging from medical oncology and radiology to plastic surgery—clinicians can harness a diverse array of perspectives when treating intricate skin cancers.
This collaborative effort means that as we figure a path through treatment options, we are not working in isolation. Instead, decisions are informed by a network of insights that can highlight subtle differences in patient response and refine treatment plans in real time. Conversations about optimizing field therapies or adjusting PDT protocols now routinely include input from experts in adjacent fields, thus improving overall outcomes.
In multidisciplinary meetings, professionals often review case studies and clinical data side by side. Such analysis enables them to poke around the nitty-gritty of treatment systems, identify potential pitfalls before they become significant issues, and refine their approach to maximize both safety and efficacy.
Key Advantages of a Cross-Functional Team Approach
- Broad Expertise: Access to specialists from various disciplines fosters a holistic view of patient care.
- Refined Decision-Making: Collaborative discussions help pinpoint the best tailored therapies for complex cases.
- Enhanced Patient Outcomes: Multidisciplinary strategies ensure that treatment plans reflect a balance between aggressive cancer control and quality-of-life preservation.
This integrated strategy not only enhances clinical outcomes but also provides reassurance for patients navigating what can be an overwhelming maze of treatment options. Knowing that their care is guided by a team of experts working together can alleviate some of the stress associated with battling skin cancer.
Future Directions: What Lies Ahead in Non-Surgical Skin Cancer Treatments
Looking forward, the horizon of non-invasive skin cancer management continues to expand. Innovations like the 10% aminolevulinic acid gel, new formulations of topical agents, and further refinements in photodynamic therapy are on the cusp of transforming how we treat superficial lesions. The anticipation around these developments is building, as preliminary data and early clinical experiences suggest that future treatments could be even more effective and less disruptive than current options.
Further research into these treatment modalities is likely to uncover additional benefits that go beyond current expectations. For instance, studies are underway to explore the combination of non-surgical therapies with emerging biologics, which could usher in an era of personalized skin cancer care. With every new clinical trial and peer discussion, we are taking a closer look at the potential of these therapies to not only treat but to also prevent skin cancers from recurring.
There remains a need for continuous innovation and research in the field. As we work through and manage our way across the evolving landscape of dermatologic care, every new piece of data adds a layer of confidence in our clinical choices. Researchers and clinicians alike are excited about the promise of these treatments, and many believe that the coming years will mark significant progress in non-surgical skin cancer care.
Trends That Are Shaping the Future
- Personalized Treatment Plans: Increasing emphasis on tailoring therapy to each patient’s unique genetic, environmental, and lifestyle factors.
- Combination Therapies: Exploring the synergies between topical agents, PDT, and biologics to optimize outcomes.
- Technological Integration: Advances in imaging and diagnostic tools that pave the way for more precise, non-invasive treatments.
- Patient Empowerment: Greater efforts to involve patients in the decision-making process, ensuring that they understand both the benefits and the potential limitations of their treatment options.
These trends signify a shift away from a one-size-fits-all mindset and toward a more nuanced, patient-specific approach. As every subtle part of treatment is continually analyzed and refined, the opportunities for improving patient care are immense. The future of non-surgical treatments in cutaneous oncology is not only promising—it is crucial for shaping a holistic framework for skin cancer care.
A Personal Perspective on the Evolution of Non-Surgical Oncology Treatments
As I reflect on the progress witnessed in the field of dermatologic oncology, I am struck by the continuous drive to merge cutting-edge science with real-world practicality. The move toward non-surgical treatment options represents a significant shift in focus—from merely eliminating tumors to considering the overall well-being of patients. For many years, the scary prospect of invasive surgeries loomed large in skin cancer treatment. Today, however, innovative approaches are emerging that enable us to treat cancers effectively while preserving the visual and functional integrity of the skin.
In my own journey as a clinician and observer of these changes, I have seen firsthand how a thoughtful balance between intervention and conservation can dramatically improve patient satisfaction. The approach is no longer only about the eradication of cancer but equally about ensuring that the methods employed do not leave behind a legacy of disfigurement. The transformation in treatment philosophy is fuelled not only by advances in technology but also by an increased sharing of knowledge through peer-to-peer learning and multidisciplinary collaboration.
It is essential for the future of dermatologic care that all parties – clinicians, researchers, and patients – stay engaged in this dialogue. As we take the wheel and make our way through the myriad treatment options available today, we must remain open to learning and adapting. Every new study, every conference presentation, and every anecdote from clinical practice has the potential to contribute to a collective wisdom that benefits all patients facing the challenges of skin cancer.
Summing Up: A Call to Embrace Change and Innovation
In sum, the exploration of non-surgical options in cutaneous oncology is not just a technical exercise—it is a paradigm shift towards more humane and patient-friendly options in skin cancer treatment. The journey is full of complicated pieces and nerve-racking decisions, but it is also rich with promise for both patients and clinicians. By focusing on tailored case studies, incorporating innovative photodynamic therapies, and eagerly anticipating the approval of groundbreaking treatments like 10% aminolevulinic acid gel, we are stepping confidently into a future where effective cancer control and cosmetic outcomes go hand in hand.
For practitioners working in this evolving landscape, it is critical to continually review the delicate balance between aggressive cancer treatment and the conservation of a patient’s natural appearance. As you steer through the tricky parts of cutaneous oncology, remember that every new twist and turn in treatment methodology is an opportunity to improve patient care. We must all commit to staying informed, participating in ongoing education, and sharing our experiences to help each other manage our way through this full-of-problems yet promising arena.
Ultimately, the progress we are witnessing reflects not only scientific advancement but also a deep commitment to patient-centered care. I invite my colleagues and readers alike to continue this conversation, to poke around the latest studies, and to bring innovative ideas from the research lab right into the consultation room. By doing so, we can ensure that the management of skin cancer remains as dynamic and compassionate as the patients we serve.
Conclusion: Steering Through the Future of Dermatologic Care
The non-surgical management of skin cancer is a clear demonstration of how innovation and practical wisdom can transform a field once thought to be rigid and unforgiving. Every step taken towards improving non-invasive treatments—whether it’s refining PDT protocols, adopting more effective topical agents, or integrating data from the latest clinical trials—represents a step towards a future where skin cancers are treated with both precision and compassion.
As we keep our eyes on the horizon, it is essential not only to welcome new therapies but also to foster collaborative efforts across specialties. When clinicians from diverse backgrounds come together to share case studies and iron out the minute details of complex treatment plans, the results benefit everyone—from the doctor’s table to the patient’s mirror.
In closing, I urge all healthcare professionals to continue taking a closer look at the evolving world of non-surgical cutaneous oncology. Let us embrace the innovative techniques that reduce the intimidating aspects of skin cancer treatment while ensuring that our approaches remain as gentle on the skin as they are effective against cancer. With informed decision-making and ongoing collaboration, the future of dermatologic care is not only bright but also beautifully balanced.
As we make our way through the shifting landscape of skin cancer therapies, every effort counts in ensuring that our patients receive care that is both state-of-the-art and deeply respectful of their quality of life. The journey may be loaded with challenges and full of tangled issues, but by steering through these turbulent waters, we pave the way for a new era in cutaneous oncology—one that is as innovative as it is compassionate.
Originally Post From https://www.dermatologytimes.com/view/navigating-non-surgical-options-in-cutaneous-oncology
Read more about this topic at
Non-Surgical Skin Tightening
7 Best Non-Invasive Beauty Treatments of 2023