Opinion: Rethinking Cancer Immunotherapy and Its Tangled Issues
The modern journey of immunotherapy in cancer treatment is as exciting as it is full of problems. Recent breakthroughs in conditionally activated immunotherapies open an intriguing chapter in our fight against cancer, especially for those battling metastatic prostate cancer. As someone who has been following these developments closely, I want to share my thoughts on how these new therapies are not only promising but also a step forward in managing the tricky parts of cancer treatment side effects.
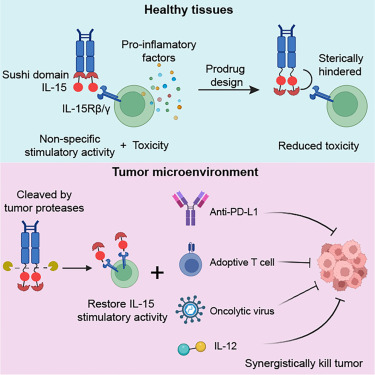
Our immune system is designed to guard against the development of cancer by constantly patrolling our bodies to eliminate unhealthy cells. Yet, when it comes to targeting cancer, the immune response can sometimes go off track, leading to unintentional damage to healthy tissue. In this editorial, I’ll take a closer look at how conditionally activated immunotherapies, specifically those targeting CTLA-4 checkpoint proteins, could offer a more refined approach that minimizes the confusing bits and unintended side effects. We will explore the design, potential benefits, and the future of these promising treatments.
Understanding Immune Checkpoint Inhibitors and Their Tricky Parts
Immune checkpoint inhibitors have been a breakthrough for cancer patients by overriding the natural brakes that prevent immune cells from attacking all cells indiscriminately. These antibodies work by blocking checkpoint proteins, such as CTLA-4, which normally help to regulate the immune response. However, as many experts have pointed out, these treatments come with their own share of tangled issues.
The key concern with conventional checkpoint inhibitors is that while they activate the immune response against cancer cells, they may also trigger immune responses against healthy tissue. This can cause a range of side effects, from rashes and diarrhea to chronic inflammation. In other words, when you unleash this powerful therapy, you might inadvertently set off a chain reaction of unintended consequences. It’s like trying to extinguish a fire with water and ending up flooding the house in the process.
Traditional CTLA-4 blocking therapies are administered intravenously, meaning they circulate throughout the body, not just targeting the tumor. Although this approach has helped many patients, it can be quite nerve-racking because of the off-target effects. This is the backdrop against which innovative strategies, such as the tumor-targeted checkpoint inhibitors developed by Dr. Larry Fong and his team, have emerged.
Tumor-Specific Immune Checkpoint Blockade in Prostate Cancer
In a groundbreaking study recently published in the Journal for Immunotherapy of Cancer, Dr. Larry Fong’s team took a fresh look at how CTLA-4 antibodies could be conditionally activated to minimize collateral damage. Their approach uses an extra cleavable domain that attaches to a prostate tumor marker, effectively turning the antibody “on” only when it reaches the tumor site. This technique is aimed at preserving the anti-cancer benefits while reducing the side effects commonly seen in traditional therapies.
Here are some key points about this innovative approach:
- Conditionally activated checkpoint inhibitors are designed to “hide” until they get to a prostate tumor, bound by tumor-specific enzymes.
- These new antibodies rely on the high levels of an enzyme called matriptase present in certain prostate tumors.
- Once in the tumor’s microenvironment, the enzyme cleaves the extra domain attached to the antibody, activating it only locally.
This tumor-specific design represents a significant turn in our efforts to sort out the fine points of immunotherapy. By ensuring that the checkpoint inhibitor activates only in the area where it is needed, researchers hope to reduce the complications of systemic immune activation.
Conditional Activation Versus Traditional Techniques: A Comparative Look
One of the most fascinating aspects of the study is the comparison between the traditional CTLA-4 inhibitors and the new conditionally activated antibodies. According to the research, the fully cleaved, conditionally activated antibody was just as effective in controlling tumor growth as the conventional therapy. However, the difference lay in the side effects observed. Mice treated with the newer, targeted version did not lose as much weight, suggesting a lower level of toxicity.
This invites us to consider the advantages of targeted treatments in a more nuanced way. When we compare the traditional versus tumor-targeted method, several subtle differences emerge:
| Characteristic | Traditional CTLA-4 Inhibitors | Conditionally Activated Inhibitors |
|---|---|---|
| Tumor Specificity | Lower; circulates systemically | High; activated only at tumor site |
| Toxicity | Higher; more side effects observed | Lower; reduced off-target damage |
| Efficacy in Tumor Control | Effective | Equally effective, as seen in controlled studies |
| Weight Loss in Preclinical Models | Significant weight loss | No significant weight loss |
This table highlights not just a technical improvement but also underscores the potential for real-world benefits in patients. For many, the side effects of cancer treatment can be as challenging as the disease itself. By reducing these effects, the conditionally activated antibodies might offer a more sustainable and patient-friendly option.
Addressing the Overwhelming Concerns of Off-Target Side Effects
Many patients and their families find the side effects of cancer treatment overwhelming. The current landscape of cancer immunotherapy is loaded with concerns about unintended damage to healthy tissues. This is especially true for CTLA-4 blockade therapies that, while targeting tumors, may also cause unwanted inflammation and other adverse reactions.
By employing a tumor-conditional activation design, we can take a more measured approach to harnessing the body’s immune defenses. Instead of a blanket activation, this method allows clinicians to figure a path through the maze of immune responses, ensuring that the treatment targets cancer cells by and large, while leaving healthy tissues as untouched as possible.
This is particularly important not just for efficacy but also for quality of life. When you reduce the side effects—be it rashes, diarrhea, or chronic inflammation—patients can focus more on recovery and less on managing competing health issues. Thus, the promise of the new immunotherapy approach extends beyond pure efficacy; it is also a promise of a gentler, more patient-centered treatment regimen.
Lessons Learned from Preclinical Studies
The research conducted by Dr. Fong’s team in preclinical models has offered several key insights. In studies with mice, the following observations were made:
- The fully cleaved conditionally activated antibody controlled tumor growth as effectively as the traditional inhibitor.
- Preclinical models indicated that mice receiving the new treatment not only showed similar survival outcomes but also avoided significant weight loss, an important marker for off-target toxicity.
- The immune profiling of treated mice revealed higher levels of activating immune cells and a decrease in repressive immune cells, both at the tumor site and systemically.
These points are critical when we consider the fine shades that differentiate an effective therapy from one that is riddled with problems. They underscore the potential of a conditional approach to eliminate some of the hidden complexities associated with current immunotherapies.
Emerging Long-Tail Keywords: Condition-Dependent Cancer Immunotherapy Benefits
The concept behind conditionally activated immunotherapies is not only innovative but also aligns with many emerging long-tail keywords in the healthcare and biotechnology sectors. As we examine this topic, it’s useful to consider some of the specific benefits:
- Improved safety profile: By preventing systemic exposure of the antibody until it reaches the tumor, the risk of damaging healthy tissue is reduced.
- Precise tumor targeting: The design relies on enzymes unique to the tumor environment, ensuring that the treatment is active only where needed.
- Potential use in metastatic cancers: Given that metastases are common in prostate cancer, the ability to target tumors throughout the body while mitigating side effects is a significant advancement.
These benefits collectively improve our overall management strategy for cancer patients, offering a promise of more personalized and less intimidating therapeutic options. As we get into the details, these condition-dependent therapies represent a compelling blend of precision and safety, which is a must-have for next-generation cancer treatments.
Dive Into the Future of Cancer Immunotherapy
There is a growing excitement among scientists and clinicians about pushing the envelope on these conditionally activated immunotherapies. Dr. Fong’s team is now considering using similar conditional activation approaches to further refine other types of immunotherapies. This presents several exciting possibilities:
- Extension to other checkpoint proteins: Imagine a future where multiple checkpoint inhibitors are tailored to work conditionally, each designed to activate only in the presence of a tumor-specific enzyme. This could dramatically reduce the risk of side effects across a range of cancers.
- Combination therapies: Pairing these targeted antibodies with other forms of cancer treatment, such as radiation or chemotherapy, may enhance overall efficacy while keeping the treatment profile manageable.
- Wider applicability in metastatic disease: Because metastases present a major challenge with current systemic therapies, having more targeted tools can help manage the tiny details of metastasis control more effectively.
The ability to direct immune responses more precisely could revolutionize cancer care. This future is not far off—research is steadily working toward refining these therapies to the point where they can reliably steer through the maze of immune responses, balancing the need for precision with the complexities of biological systems.
Patient-Centered Benefits and Real-Life Implications
While the scientific and clinical communities continue to advance our understanding of conditionally activated immunotherapies, one must not lose sight of the real-life impact these advances can have on patients. For individuals fighting cancer, improving the therapeutic index of a treatment is super important. Here are some of the most patient-centered benefits:
- Enhanced quality of life: By reducing systemic side effects such as weight loss and chronic inflammation, patients can experience fewer interruptions to their daily lives and overall well-being.
- More tolerance to treatment: Fewer side effects mean that patients may be able to stick with the treatment longer, which could improve long-term outcomes.
- Potential for outpatient administration: With a better safety profile, these therapies might be administered in more convenient settings, reducing the need for prolonged hospital stays.
- Improved survival rates: As the therapy hones in on the tumor while bolstering the immune system’s response, patients could enjoy both better cancer control and improved survival outcomes.
The real-life benefits of these condition-based immunotherapies are deeply intertwined with quality of life issues. Instead of facing a cascade of side effects that might distract from the primary goal—fighting cancer—patients can potentially experience a smoother, less intimidating journey. This shift could foster a new era of cancer care that is as supportive as it is transformative.
Managing Your Way through the Labyrinth of Modern Cancer Treatments
The emergence of conditionally activated immunotherapies invites patients, clinicians, and researchers alike to figure a path through a maze of complicated pieces that previously seemed insurmountable. The targeted activation not only represents a technological leap but also a more human approach to managing cancer treatments. Here’s a simplified breakdown of the key concepts:
- Targeted Activation: Instead of a global immune boost, these antibodies “wake up” only when they reach a specific tumor marker, cutting down on unintended adverse effects.
- Balancing Act: The new strategy works like a scale that balances effective tumor control with minimal side effects, managing the body’s immune response like steering carefully through a maze.
- Focus on Precision Medicine: By tailoring therapies to a patient’s unique tumor characteristics, we can better handle the subtle parts of cancer treatment that are critical for success.
For patients and families, this approach helps clear a path through what has often felt like an overwhelming world of choices and complications. It offers a glimpse of a future where treatments are not only more effective but also far less intimidating on a day-to-day basis.
Charting a New Course: Clinical Implications and Future Directions
The promising preclinical results of conditionally activated CTLA-4 inhibitors have far-reaching implications for how we treat not just prostate cancer, but potentially many other types of solid tumors. Here are some future directions that could be explored based on the current research:
- Expansion to Other Tumor Types: Researchers can investigate whether similar cleavage-dependent mechanisms can be applied to other cancers where specific tumor markers are present. This could open the door to broader applications in oncology.
- Combination with Other Modalities: Integrating these antibodies with existing treatment modalities, such as chemotherapy or radiotherapy, may further increase their effectiveness. Combining therapies might help overcome the fine shades and slight differences in immune responses observed among patients.
- Long-Term Outcome Studies: Conducting longitudinal studies in patients will be crucial to determine the durability of responses and overall survival benefits. Future clinical trials could provide more insight into how these condition-dependent approaches perform over extended periods.
These future directions are not just a roadmap to better therapy; they also promise greater personalization in how we approach treatment. As clinicians and researchers work together, the focus remains on turning a promising idea into a routine part of patient care—making a positive impact on countless lives.
Reflections on the Scientific Journey and Hidden Complexities
Looking back at the evolution of immunotherapy, one cannot help but be impressed by how far the field has come. The journey from broad immune activation to highly targeted, conditionally activated treatments is marked by many fine details and hidden complexities. Just a few years ago, managing the off-target effects and systemic toxicity of immunotherapies was a nerve-racking challenge. Today, with approaches such as the one pioneered by Dr. Fong’s laboratory, there is genuine hope that we can refine these strategies for improved patient outcomes.
This journey reminds us that scientific progress is often a process of refining old ideas. It involves taking a closer look at each twist and turn and seeking out small distinctions between effective and less effective methods. By digging into the details of how our immune systems interact with tumors—and how therapies can be designed to intervene only when necessary—we can feel more assured in our ability to innovate at the crossroads of biology and technology.
Weighing the Benefits and Risks: A Balanced Outlook
No discussion of advanced cancer treatments is complete without acknowledging the fine balance between benefits and risks. Like any therapeutic intervention, conditionally activated immunotherapies are not without their challenges. However, the preclinical data suggests a promising reduction in the overall risk profile. Here’s a summary of the balanced outlook on these therapies:
- Benefits:
- Targeted activation leads to lower systemic toxicity.
- Comparable tumor control to traditional therapies without the same degree of side effects.
- Greater potential for integration into combination treatment plans.
- Potentially improved quality of life for patients due to fewer off-target effects.
- Risks and Considerations:
- Long-term effects and durability of the treatment still need to be studied in clinical trials.
- There may be unforeseen challenges when transitioning from animal models to human patients.
- Optimizing the balance between complete and partial cleavage of the antibody will be critical for success.
This balanced outlook is key for patients, clinicians, and policymakers as we work together to make decisions that could impact the lives of thousands battling aggressive cancers. Understanding that every treatment option comes with its own set of tricky parts is the first step toward an informed and compassionate healthcare system.
Public Perception and the Future of Personalized Cancer Care
As advances in immunotherapy become more widely reported and better understood, public perception is sure to shift in favor of more personalized and refined treatment strategies. Many patients are tired of one-size-fits-all solutions and are eager for treatments that take into account the subtle details of their individual disease profiles. The conditional activation of immunotherapies is a prime example of how science is starting to answer those calls.
This is particularly true for those battling metastatic cancers, where the options have traditionally been limited and off-target effects are not just an inconvenience, but a serious health risk. When we are able to target tumors more accurately, the potential for more effective, less intimidating treatments grows exponentially. In turn, this can lead to better patient adherence to treatment plans, improved outcomes, and a more hopeful outlook on long-term survival.
Conclusion: A Promising Horizon in Cancer Treatment
In conclusion, conditionally activated immunotherapies represent a bold new step in the evolution of cancer treatment. By harnessing the power of the immune system in a more targeted manner, we stand at the brink of a future where the management of cancer becomes less about enduring overwhelming side effects and more about achieving sustained, quality responses.
This innovative approach tackles many of the tangled issues that have long plagued traditional immunotherapies. It demonstrates that by taking a closer look at the fine points of how our treatments interact with tumors at a molecular level, we can forge new paths toward safer, more effective therapies.
For patients, families, and clinicians, these advances offer hope—a hope that the next generation of cancer treatments will be designed not only to fight the disease but also to respect the delicate balance of the human body. In this era of personalized medicine, every small twist and subtle detail matters. As we work through the maze of modern cancer care, the future appears brighter, with treatment options that are as innovative as they are compassionate.
While we are still at an early stage in fully realizing the potential of tumor-specific immunotherapies, the momentum is undeniable. With ongoing research, expanded clinical trials, and a commitment to patient-centered care, there is every reason to be cautiously optimistic about the next chapter in cancer treatment. The breakthroughs we see today may well pave the way for tomorrow’s standard of care—a standard where targeted, conditional activation therapies offer not only effective cancer control but also a much-improved quality of life.
In reflecting on this exciting journey, I am reminded that progress in medicine is rarely linear. There are many twists and turns along the way, and the road is often full of confusing bits and nerve-racking choices. Yet, innovation is all about taking these challenges head-on and turning them into opportunities for improvement. Conditionally activated immunotherapies exemplify this transformative spirit, marking a shift towards more refined, patient-friendly cancer care.
Ultimately, the promise of this new approach is not just in its technical achievements, but in its potential to restore hope and dignity to thousands of individuals struggling with one of life’s toughest adversaries. As a committed observer and advocate for patient-centered therapies, I encourage continued dialogue, research, and collaboration across the scientific and medical communities. By staying curious and open to novel ideas, we can ensure that future cancer treatments are both cutting-edge and compassionate—a true reflection of modern medicine’s finest qualities.
Let us look forward to a future where navigating the tricky parts of cancer therapy becomes less daunting, where the complex interplay of immune cells is harnessed safely, and where every patient’s journey is met with treatments that are as effective as they are empathetic. The landscape of cancer treatment is evolving rapidly, and with it, our optimism for a future free from the heavy toll of side effects and generalized therapies. With every small advancement, we take one more step toward a holistic, patient-centered era in healthcare.
As we continue to dig into the research and explore each fine detail of new therapies, the path forward is clear: targeted, conditionally activated immunotherapies are not just a hopeful promise—they are a tangible step forward in rethinking how we fight cancer. And in the face of such innovation, both the medical community and patients have every reason to remain hopeful and engaged in the journey toward better, safer cancer care.
Originally Post From https://www.fredhutch.org/en/news/spotlight/2025/06/tst-arias-jimmunothercancer.html
Read more about this topic at
Immunotherapy: Precision Medicine in Action
Advances in Immunotherapy and Innovative Therapeutic …