Pancreatic Cancer in China: A 10-Year Look at Treatment Options and Outcomes
Pancreatic cancer remains one of the most intimidating diagnoses, challenging both clinicians and patients with its tricky parts and tangled issues. A recent 10‐year multicenter investigation in China examined treatment options, patient characteristics, and survival outcomes for those diagnosed with pancreatic cancer. This op-ed takes a closer look at the study, highlighting turning points in treatment, the impact of patient demographics, evolving chemotherapy regimens, and future directions that may help steer through the confusing bits of this deadly disease.
Early Detection and Diagnosis: The Critical First Step
One of the key findings in this investigation is that more than half of the patients were diagnosed at stage IV. This means that for the majority of patients, pancreatic cancer is discovered at an advanced phase, when it is already loaded with problems and the options for treatment are extremely limited.
Late detection of pancreatic cancer is often attributed to the disease’s subtle presentation. The symptoms may be vague, and the fine points of early clinical signs can be easily overlooked. Owing to this delay, many intricate details of the illness become blurred, and by the time of diagnosis, the tumor has often passed the window where surgical intervention is most beneficial.
Barriers to Early Diagnosis
There are several reasons why pancreatic cancer is frequently diagnosed late. Some of the most overwhelming issues include:
- Vague symptoms: Abdominal discomfort, weight loss, and digestive troubles may be casually dismissed as more common gastrointestinal issues.
- Lack of screening: Unlike other cancers, there is no widespread, standardized screening method for pancreatic cancer.
- Lack of awareness: Both the public and some healthcare providers are sometimes unaware of the subtle signs and ticking points that could hint at early disease.
As a result, medical professionals stress that improving early detection methods is essential. This is a critical step because catching the disease early could open the way for more aggressive treatment options, particularly surgical resection, which remains one of the best chances for long-term survival.
Advances in Surgical Treatment: Open vs. Minimally Invasive Approaches
Surgery remains central for patients with resectable pancreatic cancer. The investigation showed that nearly 67% of the patients received surgical treatment and among these, a commendable level of precision was observed, with 80% achieving negative margins. However, it is also important to take a closer look at the surgical techniques used.
Open Surgery and Its Limitations
Traditional open surgery dominated the surgical landscape in this study, with over 90% of procedures conducted via open approaches. While open surgery allows surgeons to make their way around the complex anatomy and perform meticulous resection, it comes with its own set of challenging bits:
- Long recovery times: Patients undergoing open surgery often face prolonged hospital stays and recovery periods.
- Higher risk of complications: Greater invasiveness means increased risk for wound infections and other postoperative issues.
- Increased blood loss: Open procedures can result in more blood loss, which is particularly challenging for patients already in a compromised state.
Embracing Laparoscopic and Robotic Surgery
The study indicated that laparoscopic surgery and the emerging use of robotic techniques were infrequently applied during the study period. However, other research and current clinical practice suggest that these minimally invasive techniques can reduce blood loss, shorten hospital stays, and lessen some of the overwhelming recovery challenges associated with traditional open surgery.
Several key benefits of minimally invasive surgery include:
- Smaller incisions: This leads to quicker wound healing and reduces infection risk.
- Finer control of surgical instruments: Robotic systems can help surgeons manage the little twists and turns of pancreatic anatomy more efficiently.
- Potential for better oncological outcomes: Despite the nerve-racking complexity, early data suggests that when executed well, minimally invasive procedures can yield comparable or even improved survival rates compared with open surgery.
Shifting from open techniques to laparoscopic or robotic approaches is not just a matter of technological adoption; it also signifies a change in how healthcare providers take the wheel in managing these complicated pieces of cancer treatment. Future research is focused on validating these benefits further and making such techniques more widely available in China and globally.
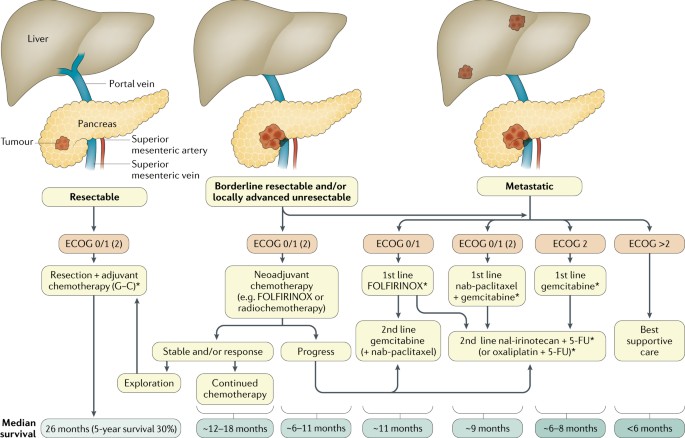
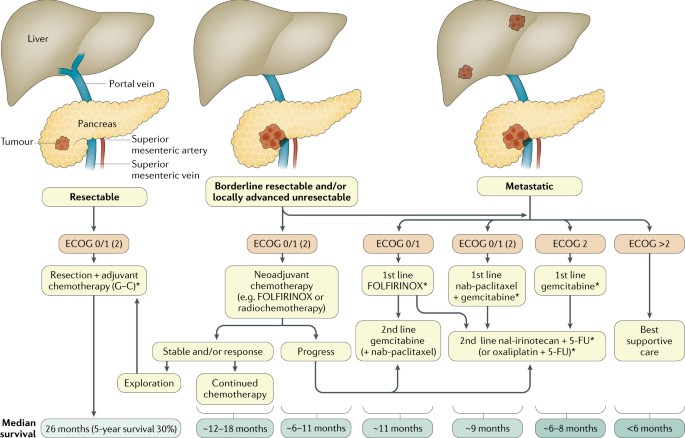
Chemotherapy Regimens: Evolving Treatments for Advanced Disease
The study also examined several chemotherapy regimens used in both the adjuvant (post-surgery) and palliative (advanced disease) settings. Chemotherapy for pancreatic cancer has seen significant reworking in recent years, and the analysis provides important insights into which combination therapies may have a stronger impact on survival compared to standard gemcitabine monotherapy.
Adjuvant Therapy: Combination vs. Monotherapy
In the setting of adjuvant therapy, which is intended to reduce the risk of recurrence after surgery, the combination of gemcitabine with fluorouracil was found to offer superior benefits over gemcitabine alone. The hazard ratios indicated a substantially lower risk of death, suggesting that a two-drug regimen might be more effective than one drug alone.
This finding is essential because the traditional approach of using a single drug (gemcitabine) might not sufficiently tackle the tangled issues that predispose patients to relapse. Optimizing chemotherapy combinations helps in reducing the overwhelming risk associated with the disease, improving survival rates for those who manage to have their tumors resected.
Advanced-Stage Treatment: First-line and Second-line Regimens
For patients with advanced pancreatic cancer, the study underlines that first-line treatment regimens using a mix of drugs, such as tegafur alone or in combination with gemcitabine and platinum-based agents, were associated with lower mortality risks when compared to gemcitabine alone. This suggests that combination therapy can reduce the risk of death among patients with late-stage disease, even if the data is based on older treatment protocols.
Second-line treatments, used when the disease becomes resistant to initial therapies, showed promising trends for FOLFIRINOX (a regimen that combines irinotecan, oxaliplatin, leucovorin, and 5-fluorouracil). Although the results were not statistically definitive due to limited sample sizes, the point estimates imply that FOLFIRINOX offers a promising way to reduce risk in the difficult-to-treat second-line setting.
Complexities in Choosing the Right Chemotherapy Regimen
Choosing an optimal chemotherapy regimen is akin to solving a puzzle full of twists and turns. Several factors need to be considered:
- Patient’s overall health: Older patients or those with a lower body mass index (BMI) may have different tolerances for intensive therapies.
- Disease stage and tumor differentiation: Late-stage tumors or those with poor differentiation often call for more aggressive treatment combinations.
- Potential side effects: The additional drugs in combination regimens might increase the risk of side effects, which can be overwhelming for both patients and clinicians.
Finding your path through these treatment options requires careful and personalized consideration. Ultimately, ongoing research and clinical trials are critical as they might introduce new drug combinations or treatment protocols tailored to individual patient profiles.
Impact of Patient Demographics on Treatment Outcomes
Another important aspect highlighted by the investigation is the role patient demographics play in treatment outcomes. Age, BMI, and even a history of conditions such as pancreatitis appear to influence survival rates. Understanding these subtle details is essential to managing the patient population as a whole.
Age: A Double-Edged Sword
The study revealed that older patients were at a higher risk of mortality. When comparing different age groups, the hazard ratios increased significantly with age. Patients aged 75 and older showed a particularly steep rise in risk, highlighting a need for more tailored approaches in elderly populations.
This pattern is especially concerning because many older patients, who may also have other competing health issues, face an intimidating treatment journey. Clinical teams must be careful to balance aggressive treatments with quality-of-life considerations of this vulnerable group.
Body Mass Index (BMI) and Nutritional Status
Interestingly, the research found that patients with a low BMI (underweight) had an increased risk of death compared to those with a normal BMI. Low body weight in the context of pancreatic cancer is often a reflection of advanced disease, where significant weight loss is common due to a combination of poor appetite, metabolic changes, and the tumor’s overall impact on body function.
This finding underscores the importance of nutritional intervention as an essential part of the treatment plan. In practice, clinicians are encouraged to work in tandem with nutritionists to provide dietary support, manage weight loss, and maintain overall health during and after treatment. The following checklist may help clinical teams manage nutritional challenges:
- Regular monitoring of weight and BMI
- Assessment of dietary intake and nutritional deficiencies
- Personalized nutritional counseling
- Consideration of supplements or nutritional support therapy
By integrating nutritional care into the overall treatment strategy, it is possible to help mitigate some of the overwhelming issues that low BMI presents.
Laboratory Testing and Tumor Markers: Uncovering Hidden Complexities
Laboratory tests such as Ki-67 and CK or AE1/AE3 immunohistochemistry offer critical insights into tumor biology. In the study, these tests were performed in only a small percentage of patients, yet among those who were tested, the positivity rates were extremely high. These markers can provide clues about the tumor’s aggressiveness and its ability to spread, which in turn can influence treatment planning.
The Role of Ki-67 in Pancreatic Cancer
Ki-67 is a marker that helps in evaluating the cell proliferation rate. In simple terms, it gives clinicians a sense of how quickly the tumor cells are growing. A higher positivity rate often indicates a more aggressive tumor behavior. However, the low testing rate observed in this study points to a missed opportunity in harnessing valuable prognostic information.
Increasing the uptake of such tests is super important because it can help physicians dig into the fine points of tumor differentiation and, consequently, adopt treatments that are better suited to the patient’s particular cancer profile.
CK or AE1/AE3 Testing for Enhanced Diagnostic Accuracy
Similarly, cytokeratin markers like CK or AE1/AE3 are used to confirm the diagnosis and study the patterns of tumor spread. The study found a high positivity rate, suggesting that when tested, these markers consistently support the diagnosis of pancreatic malignancy. Unfortunately, low rates of testing mean that many of the hidden complexities of the cancer remain unexplored in routine practice.
Moving forward, improving the frequency and comprehensiveness of laboratory testing could help clinicians figure a path toward more personalized treatment plans. Such improvement is not merely a technical detail—it is a super important measure to better predict prognosis and guide treatment decisions.
Future Directions: Lessons Learned and Paths Forward
Despite being based on data from 2005 to 2014, the study provides several crucial insights that remain relevant today. Its findings point to both achievements and underexplored areas in the treatment of pancreatic cancer in China.
Improving Early Screening and Diagnosis
One of the pressing lessons from this investigation is the need to enhance early detection programs. Increased public awareness, improved imaging techniques, and the integration of novel biomarkers into diagnostic routines may help catch pancreatic cancer at a more manageable stage.
Recent technological advances, including liquid biopsies and enhanced imaging modalities, offer hope. For instance, some research is exploring the detection of circulating tumor DNA (ctDNA) as a way to identify cancers early. Such measures could be game-changers in a field historically overshadowed by late diagnosis and confusing bits of clinical ambiguity.
Optimizing Surgical and Chemotherapy Strategies
The study underlines that surgery, when performed under optimal conditions, markedly improves survival. However, given the overwhelming challenge that most patients face at the time of diagnosis, there is a significant push toward refining surgical techniques and supporting them with well-designed chemotherapy regimens.
Some points to consider include:
- Personalized Chemotherapy: Further research is needed to chart out tailored chemotherapy protocols that account for patient age, BMI, and tumor characteristics. Combination regimens have already shown promise over monotherapy, and ongoing studies may refine these protocols even more.
- Enhanced Supportive Care: Managing treatment side effects, nutritional deficits, and emotional well-being is equally critical. Treating pancreatic cancer requires a comprehensive approach, integrating surgical prowess with supportive care measures.
- Emerging Therapies: Novel therapeutic options, including targeted therapies and immunotherapies, may soon play a larger role. While these were not common in the study period, current research suggests their potential in addressing some of the fine details of tumor biology.
These improvements in clinical strategies can help steer through the nerve-racking challenges of advanced pancreatic cancer and may ultimately lead to better survival outcomes.
Strengthening Data Collection and Research Infrastructure
The study relied heavily on retrospective data from multiple centers, an approach that has its own set of limitations—missing data, variability across institutions, and uneven use of laboratory tests. As China moves further into the digital era, there is ample opportunity to digitize patient records and create richer, more uniform databases that can provide deeper insights into treatment outcomes.
By investing in data infrastructure and conducting prospective studies, researchers can more accurately measure treatment efficacy and the impact of various risk factors. This is a super important move that will allow future analyses to dig into even the hidden complexities that might have been missed in earlier investigations.
Addressing the Overarching Challenges in Pancreatic Cancer Treatment
Although this 10-year study offers several promising insights, pancreatic cancer continues to be a disease riddled with issues—from late diagnosis to complicated treatment decisions. Both clinicians and policymakers must recognize that effective management approaches involve a multi-pronged strategy that includes:
- Early detection and awareness: Investing in public health campaigns and professional education to ensure that early signs of pancreatic cancer are not missed.
- Diverse treatment modalities: Encouraging the adoption of both traditional and cutting-edge surgical techniques as well as advancing chemotherapy protocols.
- Personalized patient care: Acknowledging that patient demographics, such as age and nutritional status, significantly impact treatment response, and tailoring therapies accordingly.
- Enhanced laboratory testing: Increasing the frequency and detail of tumor marker testing to better guide treatment decisions.
- Robust data collection: Moving toward standardized, digital record-keeping to ensure that future research can capture the subtle parts of pancreatic cancer trends.
By addressing these pressing challenges head-on, the medical community can begin to untangle the confusing bits and make real strides in reducing mortality rates. While the current research is based on data that is several years old, the lessons it offers remain applicable today as the field continues to evolve.
Conclusion: A Path Forward in Pancreatic Cancer Care
The 10-year multicenter study on pancreatic cancer treatment options in China provides a valuable window into the state of care for one of the most overwhelming malignancies. With an emphasis on late diagnosis, the study reveals that more than half of patients face an overwhelming battle at stage IV, making early detection and timely intervention a critical area of focus.
Surgical care in China has advanced, with high rates of negative surgical margins showing promise. Yet, the reliance on open surgery, as opposed to minimally invasive approaches, points to an opportunity for improvement. Likewise, the study’s insights into chemotherapy, particularly the benefits of combination regimens in both adjuvant and advanced disease settings, pave the way for more tailored therapeutic approaches.
Patient demographics, such as age and BMI, are shown to have a significant impact on outcomes, underscoring the need for personalized treatment plans. Laboratory testing for crucial tumor markers like Ki-67 and CK/AE1/AE3, though currently underutilized, holds potential for refining prognosis and guiding treatment strategies.
To truly take control of the tangled issues in pancreatic cancer care, efforts should concentrate not only on improving early diagnosis and treatment options but also on upgrading data collection and research methodologies. By doing so, the medical community can figure a path toward more personalized and effective treatment strategies—a move that is super important for ultimately reducing the high mortality rates associated with this challenging disease.
Looking forward, continued innovation, research, and coordinated care will be the cornerstones of progress. By improving early detection methods, embracing minimally invasive surgical techniques, refining chemotherapy protocols, and personalizing treatment based on patient characteristics, we can hope to turn the tide in the battle against pancreatic cancer.
This op-ed serves as both a reflection on past efforts and a call to action for the future. The healthcare community, policymakers, and researchers must work together to address these overwhelming challenges—one tricky part at a time—to ensure that patients battling pancreatic cancer receive the comprehensive, effective care they deserve.
Originally Post From https://www.wjgnet.com/1948-5204/full/v17/i8/106447.htm
Read more about this topic at
Pancreatic Cancer Treatment (PDQ®)
Advances in pre-treatment evaluation of pancreatic ductal …