Olanzapine and Its New Role in Managing Chemotherapy-Induced Nausea in Breast Cancer
Breast cancer treatments have made significant strides over the years, yet the tricky parts of managing side effects from potent chemotherapy regimens remain a major concern. One of the most intimidating aspects of chemotherapy is dealing with nausea and vomiting. A recent phase 3 trial has sparked interest by demonstrating that a combination of 5 mg olanzapine, when added to a triplet antiemetic therapy, offers markedly better control of chemotherapy-induced nausea and vomiting (CINV) for patients with breast cancer.
This editorial will take a closer look at the new findings, discuss the benefits of using olanzapine in combination with traditional agents, and explore the potential impact on patient care. We will also look into the detailed design of the trial and the outcomes that could influence clinical practice. By examining the results and considering the broader context, we hope to provide insights into how this strategy can improve the quality of life for patients undergoing treatment.
Enhanced Control of Chemotherapy-Induced Nausea and Vomiting in Breast Cancer Patients
For patients initiating anthracycline plus cyclophosphamide-based chemotherapy, the onset of nausea and vomiting can be a nerve-racking experience. The new evidence stems from a rigorously conducted randomized, double-blind, placebo-controlled trial. In this study, patients who received the 5 mg olanzapine addition to the triplet antiemetic regimen reported not only better nausea control but also higher overall satisfaction with the treatment.
The trial involved patients with stage I to III breast cancer who were at high risk for experiencing CINV. The treatment regimen included a NK-1 receptor antagonist, palonosetron (a serotonin receptor blocker), and dexamethasone. With the olanzapine group showing a complete response (CR) rate of 58.1% over 168 hours compared to 35.5% in the placebo group, the stark differences suggest that even a modest dose of olanzapine can dramatically ease the rough-edged experience of chemotherapy.
Key Findings and Their Impact on Clinical Practice
One of the highlights of the trial was the notable difference in the time to treatment failure. In the olanzapine arm, the median time to failure was not reached, compared to 37.3 hours for the placebo group. This indicates that patients taking olanzapine were able to sustain relief for a longer period. Medical practitioners who work through the tricky parts of supportive care for cancer patients will find that this improvement could reshape the way antiemetic regimens are structured.
Moreover, the increased satisfaction scores observed among patients in the olanzapine group underline the importance of addressing not just the physical, but also the emotional distress often associated with severe nausea. For many patients, the day-to-day management of side effects is full of problems and stressful moments. Improving antiemetic efficiency, therefore, becomes a key area in making the overall treatment process less overwhelming.
Combination Therapy: The Triplet Anti-Emetic Regimen Explained
When you take a closer look at the trial’s design, you see that each patient received a well-structured course of chemotherapy with combined drugs. The triplet therapy included a NK-1 receptor antagonist, highly effective in blocking pathways associated with nausea, palonosetron for its longer half-life and better receptor affinity, and dexamethasone to help reduce inflammation and nausea.
If you compare this multi-agent strategy to single-agent therapy, the difference is immediately evident. The benefits of a combination therapy include:
- Extended Duration of Protection: The use of several antiemetic agents addresses various pathways involved in nausea, thereby enhancing overall protection.
- Improved Quality of Life: Managing symptoms more effectively means that patients can focus on their recovery without the constant distraction of overwhelming side effects.
- Higher Patient Satisfaction: As demonstrated in the trial, patients receiving the multi-drug regimen showed higher satisfaction, which is crucial for adherence and overall psychological well-being during treatment.
The integration of olanzapine into this regimen adds another layer of benefit by targeting certain receptors not covered by the other agents. This factor appears to account for a significant portion of the observed improvements.
Delving Into the 5 mg Olanzapine Dosage: A Closer Look at the Details
The decision to utilize a 5 mg dose of olanzapine was made with patient safety and efficacy in mind. Traditionally known for its role in psychiatric conditions, olanzapine has been repurposed in this setting because of its antiemetic properties. The trial avoided the heavier sedation effects often seen with higher doses, ensuring that patients experienced fewer complications related to severe drowsiness.
When you pok around the fine points of the trial data, you notice:
- Patient Age and Performance: The median age was similar between groups, and almost all patients had an ECOG performance status of 0, indicating they were fully active prior to treatment. This uniformity helps strengthen the study’s conclusions.
- Regimen Consistency: The majority received similar chemotherapy protocols (epirubicin plus cyclophosphamide being one of the most common), ensuring that the results were not skewed by regimen variability.
- Sustained Efficacy Over Time: Both the acute phase (first 24 hours) and the extended delayed phase (24 to 168 hours) showed significant benefits, reinforcing the duration of the antiemetic effect contributed by olanzapine.
This detailed analysis demonstrates that, even when considering the small twists and turns of side effect management, a carefully chosen olanzapine dose can yield significant benefits without introducing additional complicated pieces into the patient care plan.
Comparing Olanzapine with Other Antiemetics in Cancer Care
Recently, many clinicians have been diving in to compare traditional antiemetic protocols with emerging therapies. While olanzapine is not new to the arena of psychiatric care, its application in oncology, specifically for managing CINV, offers a refreshing perspective. The data suggest that olanzapine might be a better option for patients who have historically struggled with the confusing bits of standard antiemetic therapy.
Let’s consider some advantages:
- Enhanced Patient Experience: Patients on olanzapine report feeling significantly better overall with fewer interruptions to their daily routine. This enhancement in quality of life is super important as it directly impacts treatment adherence.
- Longer Protection Period: As mentioned earlier, the time to treatment failure is prolonged, meaning that patients can enjoy longer relief between doses. That difference is essential when trying to manage the overall treatment course’s intensity.
- Minimal Additive Side Effects: At the 5 mg dosage, olanzapine did not present severe sedative side effects, which is often a concern with higher doses or with other antipsychotic drugs used in similar protocols.
Furthermore, these gains are achieved without the trade-offs typically seen when trying to balance efficacy against quality of life. This unique balance enhances the attractiveness of olanzapine as a candidate for broader use in antiemetic protocols within oncology.
Looking at the Broader Impact: Reassuring Both Clinicians and Patients
The new trial findings do more than just demonstrate a statistical improvement in nausea control – they serve as reassurance for both clinicians and their patients. For healthcare providers dealing with the tangled issues of supportive cancer care, the challenge has always been to find a treatment that is both effective and minimally disruptive.
Patients, on the other hand, are often concerned about the overwhelming side effects of chemotherapy. The reassuring data on olanzapine, particularly its ability to extend the time to treatment failure, means that for many, the intended treatment regimen becomes not only more effective but also less nerve-racking on a day-to-day basis.
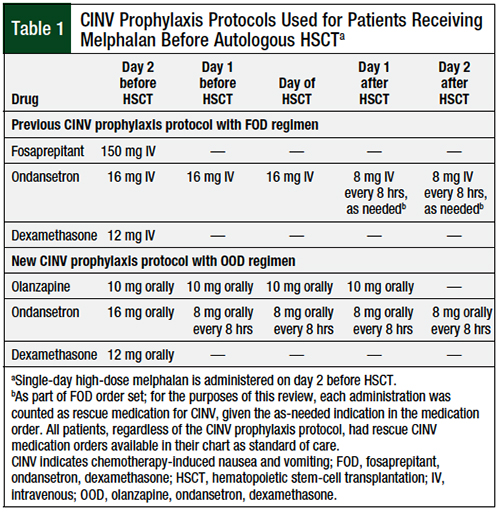
The following table provides a concise overview of the key outcomes observed in the trial:
| Outcome | Olanzapine Group | Placebo Group | Notes |
|---|---|---|---|
| Complete Response Rate (0-168 hrs) | 58.1% | 35.5% | Clear improvement over the full observation period |
| Acute Phase Response (0-24 hrs) | 76.4% | 55.6% | Early protection against emesis |
| Delayed Phase Response (24-168 hrs) | 62.9% | 41.5% | Consistently better control after first 24 hours |
| Time to Treatment Failure | Not reached | 37.3 hrs | Significantly longer sustained protection |
These figures illustrate just how impactful olanzapine can be when integrated into a properly timed and balanced antiemetic strategy.
Addressing Concerns: Side Effects and Patient Safety
Naturally, the use of any additional medication brings with it concerns about potential adverse side effects. In this trial, the safety profile of the 5 mg olanzapine dosage was carefully monitored. Despite findings of some mild side effects such as anorexia and constipation, these were notably less severe when compared to the placebo group. Moreover, the incidence of grade 3 to 4 adverse effects such as somnolence or concentration impairment was minimal.
Clinicians are often caught between the need for effective symptom management and the risk of adding medications that might introduce more complications. The study’s results help dispel some of these worries by demonstrating that the inclusion of olanzapine did not lead to any severe sedative effects or treatment-related deaths. This balance between beneficial effects and manageable side effects is critical when figuring a path through the tricky parts of supportive care.
To help organize these observations, here is a bulleted summary of the safety findings:
- Anorexia: Occurred less frequently in the olanzapine group compared to placebo.
- Constipation: Reported rates were slightly lower in the olanzapine arm.
- Somnolence and Concentration Issues: Minimal incidences observed, with no cases reaching a life-threatening severity.
- No Treatment-Related Fatalities: A critical reassurance for both clinicians and patients.
Implications for Future Research and Practice
The promising results from this trial open up several avenues for further exploration. Future research could look into optimizing the timing and combination of these antiemetic agents while considering individual patient factors such as age, overall health, and the specific chemotherapy regimen used. There is also room to explore whether similar benefits could be observed in other cancers where the chemotherapy-induced symptom burden is similarly nerve-racking.
Among the small distinctions that researchers and clinicians need to consider are:
- Differential Response Based on Chemotherapy Type: While the current study focused on anthracycline plus cyclophosphamide regimens, how might patients receiving other types of chemotherapy respond?
- Long-Term Patient Outcomes: Although immediate effects on nausea and vomiting are encouraging, there is room to study the long-term impact on quality of life and overall treatment adherence.
- Personalized Therapy Adjustments: The possibility of tailoring the olanzapine dose depending on patient tolerance could help mitigate any lingering side effects while maximizing benefit.
The subtle parts of this research underscore the importance of patient-centered care that doesn’t just zero in on shrinking tumors but also focuses on keeping daily life as normal as possible during rigorous treatments.
Integrating Research Findings into Everyday Oncology Practice
The translation of clinical trial results into everyday practice is often full of twists and turns. Healthcare teams must find ways to get around the confusing bits of integrating new protocols into established treatment regimens, especially when the stakes are so high. Oncologists, nurse practitioners, and support staff are all pivotal in ensuring that interventions like the olanzapine-enhanced antiemetic regimen are introduced safely and effectively.
Practical steps for integrating these research findings include:
- Training and Education: Ensuring all oncology staff are well-versed in the updated protocols and understand the benefits and potential side effects.
- Patient Counseling: Taking extra time to explain how the new regimen works, what improvements to expect, and how it might ease the nerve-racking side effects of chemotherapy.
- Monitoring and Feedback: Implementing robust systems to monitor patient responses and adjust dosing if necessary to maintain an optimal balance between efficacy and safety.
Incorporating these measures can help the medical community find your way through the sometimes overwhelming process of adopting and standardizing promising new practices.
Balancing Efficacy with the Challenges: The Fine Points of Supportive Care in Oncology
It is essential to recognize that while the primary focus in oncology is on treating the disease itself, supportive care plays an equally super important role. For many patients, the side effects of chemotherapy can be as debilitating as the cancer diagnosis. A well-rounded approach that includes effective antiemetic therapy can make treatment less intimidating and help patients maintain their nutritional status, mental well-being, and overall quality of life.
This trial is an important reminder that even small adjustments in supportive care can have a large impact. The addition of olanzapine into the antiemetic mix addresses several of the little twists that often make the management of chemotherapy complicated. It offers a way to reduce the frequency and severity of nausea and vomiting, which, in turn, leads to a smoother treatment experience.
Patient-Centered Perspectives: Improving Daily Life During Chemotherapy
From the patient’s point of view, the battle against cancer is as much about managing the side effects as it is about controlling the disease. The overwhelming nature of chemotherapy-induced nausea and vomiting can sap a patient’s energy and willpower, making days feel longer and more trying. The new findings might help patients regain some control over their daily lives.
For those experiencing the nerve-racking rollercoaster of chemotherapy side effects, the morale boost offered by an improved antiemetic regimen is invaluable. Many patients have shared that when the physical symptoms are managed effectively, they feel better equipped to engage in supportive activities—be it nutritional counseling, gentle exercise, or even simply enjoying time with loved ones.
Key aspects from a patient-focused perspective include:
- Empowerment Through Control: Knowing that there is an effective preventative measure against nausea and vomiting reinforces patient confidence in their treatment plan.
- Improved Mood and Energy Levels: With fewer interruptions from severe symptoms, patients can participate more fully in both their personal and social lives.
- Enhanced Communication With Providers: When patients experience fewer side effects, conversations between healthcare providers and patients about overall well-being tend to be more focused and constructive.
This improvement in overall quality of life underscores the need for medical teams to prioritize supportive care measures that address both the physical and psychological challenges of cancer treatment.
Addressing the Communication Challenge: Educating the Community
Effective communication between healthcare providers and their patients is crucial when introducing any new treatment regimen. While research findings provide the necessary data, the real challenge lies in translating that data into everyday language that patients can easily understand. The details surrounding antiemetic protocols, dose adjustments, and managing side effects can sometimes feel loaded with issues and may seem too intimidating to grasp fully.
Here are some strategies to manage your way through these communication challenges:
- Simplify the Scientific Jargon: Use clear and relatable language when discussing treatment plans. For instance, rather than saying “intricacies,” it might be better to mention “fine points” or “little details.”
- Utilize Visual Aids: Diagrams, charts, and tables can be extremely helpful in illustrating how a treatment regimen works and what benefits can be expected.
- Encourage Questions: Creating a supportive environment where patients feel comfortable asking questions helps to address the subtle details that might otherwise be misunderstood.
By working through the nerve-racking communication challenge carefully, providers can ensure that patients are well-informed and capable of actively participating in their treatment decisions.
Integrating Findings Into a Holistic Health Approach
The emerging evidence supporting the 5 mg olanzapine addition to a triplet antiemetic regimen is not just promising for the development of better supportive care practices in oncology—it also aligns with a broader shift toward holistic health approaches in medicine. Today’s healthcare landscape is increasingly recognizing the interplay between effective cancer treatment and the necessity of maintaining a patient’s overall well-being.
Integrating these findings into practice sees benefits across several dimensions:
- Better Treatment Adherence: With fewer side effects, patients are more likely to complete their full course of chemotherapy.
- Improved Mental Health: Reduced nausea and vomiting lessen the psychological strain on patients, contributing to improved mood and resilience.
- Nutritional Support: Effective management of gastrointestinal side effects means that patients can maintain better nutrition, which is critical for recovery and overall strength.
This holistic perspective is key to treating cancer, where every aspect—from tumor management to day-to-day comfort—comes together to shape patient outcomes. Finding your way through the tangled issues of cancer care requires a multifaceted approach that addresses both the disease and the person living with it.
Final Thoughts: A Step Forward in Optimizing Supportive Care
The journey toward better supportive care in oncology is often full of twists and turns, yet it is heartening to see initiatives that focus on making life more bearable for those facing the challenges of chemotherapy. The promising role of 5 mg olanzapine added to a triplet antiemetic regimen marks a significant step forward. Not only does it extend protection against nausea and vomiting, but it also empowers patients to manage their side effects better, transforming what was once an overwhelming obstacle into a manageable part of their treatment journey.
As clinicians, we must continue to figure a path through the confusing bits and tangled issues of cancer therapy. Each incremental improvement, whether in the form of simplified antiemetic protocols or more effective management of side effects, contributes to a larger picture—a picture of holistic, patient-centered care that addresses the full spectrum of challenges faced by those affected by cancer.
The lessons from this trial remind us that supportive care is as super important as the core oncologic treatments themselves. By working together, healthcare teams can sort out the delicate balance between aggressive cancer treatment and maintaining the quality of everyday life for patients. The evidence supports the effectiveness of olanzapine in a real-world scenario, and it encourages us to continue exploring novel ways to enhance the overall cancer care experience.
Looking Ahead: Future Directions in Cancer Supportive Care Research
Looking ahead, several areas stand out as ripe for further investigation and clinical refinement. Researchers need to take a closer look at the long-term outcomes of patients who receive olanzapine as part of their antiemetic regimen. Additionally, studies might benefit from exploring:
- Variations in Chemotherapy Regimens: Evaluating the efficacy of olanzapine-based protocols in patients undergoing different chemotherapy treatments could open doors to broader applications.
- Patient-Reported Outcomes: Focusing on real-world data regarding quality of life and daily functionality will provide deeper insights into the true impact of enhanced antiemetic therapies.
- Cost-Effectiveness Analyses: With healthcare costs always a consideration, determining whether this regimen can reduce overall treatment costs by reducing hospitalizations or unscheduled care visits is vital.
A combined focus on these areas will enable healthcare providers to get into a more nuanced understanding of how best to tailor supportive care regimes to individual patient needs. The intention is clear: to work through the challenging parts of treatment while ensuring that patients feel supported, both physically and emotionally.
Conclusion: The Power of Incremental Improvements in Patient Care
In closing, the integration of olanzapine into the antiemetic strategy for patients undergoing anthracycline plus cyclophosphamide-based chemotherapy for breast cancer is a promising advancement. This new approach addresses many of the nerve-racking aspects of treatment-related nausea and vomiting and provides a practical, effective solution that can radically improve patient satisfaction and quality of life.
The trial’s findings reinforce the idea that even modest changes in medication dosing and regimen design can lead to substantial gains in patient comfort and treatment adherence. For healthcare teams working on the fine points of day-to-day cancer care, these results offer a welcome opportunity to reframe their approach to supportive care.
As we continue to explore and adapt new treatment strategies, let us remember that every small improvement—every little twist that reduces the burden of treatment—counts. The enhanced antiemetic efficacy exhibited by 5 mg olanzapine, when paired with a well-established triplet regimen, marks an important milestone in the ongoing quest to offer more patient-friendly treatment options in oncology. It is a reminder that, by continually refining our methods and connecting robust clinical research with everyday practice, we can truly make a difference in the lives of those we treat.
Ultimately, the journey toward comprehensive cancer care is about finding your way through the tangled, intimidating, yet ultimately surmountable challenges that arise during treatment. With the continued collaboration of researchers, clinicians, and patients alike, we can look forward to a future where supportive care is not an afterthought but a central, empowering element of cancer treatment.
As we stand at the intersection of cutting-edge research and patient-centered care, it remains our duty to stay informed and agile. Embracing innovations such as the olanzapine-based antiemetic regimen is not just a step forward in the management of chemotherapy-induced nausea—it is a stride towards a future where every patient can face their treatment with greater confidence and less fear.
Originally Post From https://www.oncnursingnews.com/view/olanzapine-triplet-cuts-chemo-induced-nausea-vomiting-in-breast-cancer
Read more about this topic at
Nausea & Vomiting: Causes & Treatment
How to Get Rid of Nausea: 18 Methods To Try