Overview of Later-Line Metastatic Colorectal Cancer Treatment Options
Metastatic colorectal cancer (CRC) presents a challenging clinical landscape, especially in later treatment lines. As patients progress through multiple rounds of therapy, the available options become more limited and often come with tricky parts that require careful decision-making. In this opinion editorial, we’ll take a closer look at the current strategies, highlighting the benefits of rapid molecular profiling, the role of liquid and tumor biopsies, and the pros and cons of anti-EGFR rechallenge. We will also explore biomarker-driven treatment schemes to help both clinicians and patients figure a path through these tangled issues.
Rapid Molecular Profiling: The Power of Liquid Biopsy and Tumor Analysis
One of the key advances in treating metastatic CRC is the utilization of molecular profiling to guide therapy. By using both liquid biopsy (to detect circulating tumor DNA or ctDNA) and traditional tumor biopsies, physicians gain valuable information that can help guide treatment decisions promptly. While tumor biopsies offer detailed insights into the cancer’s biology, liquid biopsies can provide results rapidly, which is especially critical when there is no time to wait for traditional next-generation sequencing (NGS) results.
Benefits of Liquid Biopsy in Clinical Decision-Making
Liquid biopsies have become a super important tool in the management of later-line CRC therapy. They offer several advantages:
- Speed: Results are returned quickly, allowing for timely adjustments in the treatment plan.
- Minimal invasiveness: As a simple blood test, it is less intimidating and safer for the patient.
- Dynamic monitoring: Liquid biopsies enable clinicians to track changes in tumor genetics over time, making it possible to capture subtle details that might arise during treatment.
For example, when there is a mixed treatment response in colon cancer cases, some physicians use carcinoembryonic antigen (CEA) levels alongside ctDNA tracking to get a more accurate picture of the tumor’s activity. Although results from liquid biopsy need to be interpreted with care, they can serve as strong early predictors, especially in cases where immunotherapy may have a big impact.
Integrating Tumor Biopsy for a Complete Profile
Despite the speed of liquid biopsies, the substantial bulk of tumor tissue still holds key information that liquid biopsy might miss. At major centers like MD Anderson, the practice is to perform both types of biopsies when possible. This two-pronged approach ensures that clinicians are not just relying on a single marker or a narrow set of molecular data, but rather embracing a larger view of the tumor’s genetic landscape.
By combining the fine details obtained from the tumor biopsy with the rapid feedback from ctDNA measurements, treatment teams can fine-tune therapy selection. This is particularly helpful when managing tricky issues like identifying rare mutations or confirming if a prior treatment strategy remains valid.
Biomarker-Driven Therapies: Small Genes, Big Impact
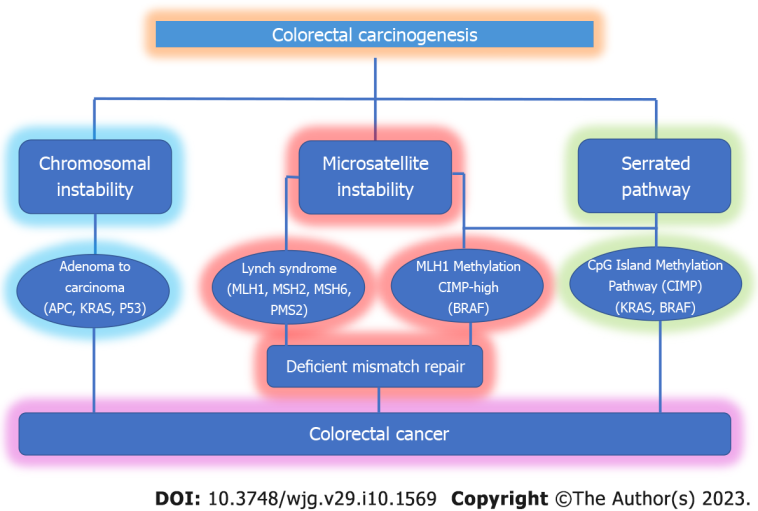
Modern treatment for metastatic CRC is highly driven by biomarkers. Knowing a tumor’s biomarker status—like RAS, BRAF, HER2, and even rare fusions such as NTRK—is critical in the selection of therapies for later lines. In the case under consideration, a patient’s tumor was identified as microsatellite stable (MSS) with no RAS, BRAF, or HER2 alterations. This information directly affects treatment eligibility and helps tailor subsequent lines.
Understanding the Impact of Rare Mutations
Even though mutations such as KRAS G12C and NTRK fusions occur in only a small percentage of cases, they signal tiny twists that require the treatment team to adjust the plan. For instance, KRAS G12C mutations, which are found in about 3% of CRC patients, may open the door for targeted inhibitors that specifically counteract the mutation’s effects. Similarly, NTRK fusions—though seen in fewer than 1% of MSS patients—might offer an alternative route for therapy provided that microsatellite instability (MSI) is present.
Role of Immune Checkpoint Inhibitors and CTDNA Monitoring
Beyond purely genetic markers, the use of immunotherapy (IO) has gained ground, especially when using ctDNA as an early readout. There is a growing body of evidence suggesting that tracking ctDNA levels can help predict response to IO treatments. This method of dig into the fine points of tumor behavior may probe for early signs of both benefit and potential pseudo-progression—a phenomenon where tumors initially appear larger due to immune cell infiltration before showing a true response to treatment.
When evaluating a patient’s profile, it becomes super important to look at how these markers change over time. Tracking ctDNA, when paired with other tumor markers like CEA, gives clinicians a more nuanced insight into how a patient is faring over several cycles of therapy.
Third-Line Options: Weighing Cytostatic Versus Cytotoxic Treatments
After patients progress through first- and second-line treatments, often with combinations like folinic acid/fluorouracil/oxaliplatin/bevacizumab and folinic acid/fluorouracil/irinotecan/cetuximab, the available choices narrow down. Therapies in the third line include agents like trifluridine/tipiracil, regorafenib, and fruquintinib. Each of these offers benefits in terms of disease stabilization, and they play a super important role, especially when radiologic responses have been mixed.
Anti-EGFR Rechallenge: A Response-Driven Approach
Among the options in later lines, anti-EGFR rechallenge is one strategy that merits special attention. This approach, which involves reintroducing an EGFR inhibitor like cetuximab after a treatment break, can sometimes yield responses even when previous treatment lines have been exhausted. The premise is that if a patient’s tumor does not harbor persistent mutations—specifically MAP kinase pathway alterations—an anti-EGFR rechallenge might generate a tumor response.
Small randomized studies have shown response rates of up to 20% for EGFR rechallenge in selected patients. For patients who truly need a response rather than mere disease stabilization, this option might be a welcome consideration. It provides a means to stimulate a cytotoxic response rather than relying solely on cytostatic agents that may extend survival without shrinking tumor size.
Making the Right Choice in Third-Line Therapy
When faced with multiple treatment options, having a clear reading of the patient’s biomarker profile is essential. For example, if the patient has already been exposed to EGFR-targeted drugs and has progressed from that therapy, it’s crucial to ensure that molecular tests—potentially via a liquid biopsy—do not show continuing signs of downstream mutations that would render the rechallenge ineffective.
This precise mapping of small distinctions in tumor biology helps clinicians ‘find their way’ through the tangled issues encountered in later-line metastatic CRC. The ultimate goal is to pick a regimen that not only provides disease control but also offers the probability of a measurable tumor response when needed the most.
Side Effects, Tolerability, and Quality of Life Considerations
The journey through metastatic CRC is not only marked by the challenge of choosing the right treatment but also by the management of treatment-related side effects. The patient mentioned in the case study experienced troublesome peripheral neuropathy, skin rash, and intermittent fatigue, which impact quality of life. Balancing treatment efficacy with toxicity remains a nerve-racking aspect of later-line management.
Monitoring and Managing Side Effects
It is vital that clinicians keep close watch on patient symptoms through routine blood tests and clinical evaluations. For instance, episodes of myelosuppression (as noticed through low white blood cell counts and platelets) or liver enzyme alterations demand regular monitoring and timely interventions. Adjustments, such as dose reductions or the introduction of supportive care measures, can help carb down the more complicated side effects of these regimens.
Individualized treatment regimens that take a patient’s history into account—like the control of pre-existing conditions such as hypertension and type 2 diabetes—are super important. Especially since the treatment itself can add to a patient’s overall burden, leading to off-putting complications if not managed carefully.
The Role of a Multidisciplinary Approach
Given the multifaceted nature of metastatic CRC treatment, a multidisciplinary approach can be the key to navigating the small twists of approach in patient care. This includes collaboration among oncologists, radiologists, pharmacists, and supportive care teams. Regular case-based review meetings, involvement in clinical trials, and adherence to guidelines from authorities like the NCCN help clinicians make well-informed decisions.
Understanding the Economic Implications of Molecular Profiling
While comprehensive molecular testing can play a super important role in tailoring therapy, the economic factors associated with such tests add another layer of tricky parts to the decision-making process. Liquid biopsies, though fast and efficient, may come with a higher upfront cost, which might not be accessible in all healthcare settings.
Cost Versus Benefit in Molecular Testing
Policymakers and clinicians alike must balance financial constraints with the undeniable benefits of rapid, detailed molecular profiling. In academic centers with significant research budgets, using both tumor and liquid biopsy methods might be the norm. However, in community practices, decisions might need to be tailored based on local availability and cost-effectiveness.
Decision trees that incorporate factors such as patient performance status, treatment history, and anticipated results from molecular testing can help guide these economic considerations. A table summarizing common biomarkers in CRC and associated treatment decisions can offer practical guidance:
| Biomarker | Prevalence in CRC | Treatment Implications |
|---|---|---|
| RAS (Wild Type vs Mutant) | Common | Eligibility for anti-EGFR therapies |
| BRAF | Moderate | Indicates poor prognosis; may guide targeted inhibitors |
| HER2 | Less common | May qualify for anti-HER2 treatment options |
| KRAS G12C | Rare (around 3%) | Potential for targeted KRAS inhibitors |
| NTRK Fusion | Extremely rare | Eligibility for specific TRK inhibitors |
By visualizing data in a clear, accessible format, both clinicians and patients can better understand the cost and benefits of each molecular test and how it may influence treatment outcomes.
Future Directions in Cost-Effective Oncology Care
As technology evolves, there is growing hope that costs for rapid molecular profiling will decrease over time, making these must-have tests more accessible to a broader patient population. Advances in automated analysis and integrated diagnostic workflows could streamline both the laboratory and clinical processes. This could eventually result in a more consistent and financially viable approach to personalized treatment in metastatic CRC.
Impact on Patient-Physician Relationships and Shared Decision-Making
One of the less frequently discussed but absolutely critical aspects of later-line treatment is the impact on patient-physician relationships. As patients face overwhelming treatment histories and experience mixed responses, it becomes essential for both parties to work through a shared treatment strategy. Open dialogues about the tricky parts of different regimen options, expected side effects, and realistic treatment goals are super important for maintaining trust and engagement in care.
Communication as a Cornerstone
Clinicians need to “take the wheel” when it comes to explaining the treatment plan clearly. This involves using plain language to describe the range of possible outcomes, including the possibility of achieving cytotoxic responses through options like EGFR rechallenge versus more gentle, cytostatic approaches. Such conversations allow patients to be strong advocates for their own care, making it easier to steer through the tangled issues presented by advanced disease.
- Setting realistic expectations: Discussing potential outcomes helps manage the immediate fears associated with side effects and treatment fatigue.
- Regular feedback: Continual monitoring and open channels of communication help adjust treatment goals as needed.
- Empowering patients: Engaging in routine discussions about molecular testing and personalized therapies can give patients the confidence to partner fully in their care decisions.
From Confusion to Confidence
It’s not uncommon for patients to feel overwhelmed by the nerve-racking array of treatment choices. By explaining the rationale behind specific molecular tests, and describing how these results impact therapy choices, physicians can help demystify the process. This clear explanation makes what might initially seem like confusing bits far more understandable, transforming uncertainty into a partnership grounded in trust and knowledge.
Assessing the Evidence: Clinical Trials and Emerging Data
As with all cancer treatment strategies, the backbone of modern metastatic CRC care is built on robust data from clinical trials. Studies exploring techniques like anti-EGFR rechallenge, the utility of liquid biopsy versus traditional tumor biopsy, and the efficacy of targeted agents provide a roadmap for care. However, these data sets often include small randomized trials, leaving some of the finer points of treatment up for debate.
Evaluating Small Trials and Real-World Data
Many of the strategies we see in later-line treatment, such as anti-EGFR rechallenge, are based on smaller studies or data extrapolated from broader population experiences. This research shows promise – for instance, some trials have noted response rates upward of 20% with rechallenge strategies in carefully selected patients.
While the sample sizes in these studies can be intimidating for some, they still provide super important insights that guide clinical decisions. Real-world data from broader patient populations further affirm the potential benefits of combining molecular testing with treatment adjustments. Clinicians must be prepared to dig into these studies and extract the nitty-gritty details that can inform practical, everyday treatment planning.
How Ongoing Trials May Change the Landscape
Several ongoing clinical trials continue to explore new avenues of treatment in metastatic CRC. Some trials focus on optimizing immunotherapy when combined with molecular profiling, while others look to enhance the efficacy of existing agents through innovative dosing strategies or combination therapies.
These emerging data sets often shed light on small distinctions between patient responses that can make all the difference in individual outcomes. As more robust studies are published, clinicians can refine treatment algorithms and possibly extend the arsenal of available therapies for those reaching later treatment lines.
Personalized Medicine: The Future of Metastatic CRC Care
Embracing personalized medicine is more crucial now than ever. The patient case considered—a 58-year-old with a history of controlled co-morbidities and prior exposure to several treatment lines—illustrates well the super important role that individualized therapy plays in metastatic CRC. By tailoring therapy based on detailed molecular and clinical profiles, oncologists can identify the most promising treatment avenues and minimize unnecessary toxicity.
Why Personalized Approaches Are Super Important
Personalized therapy offers several advantages in addressing the myriad of tangled issues present in advanced disease treatment:
- Optimized Treatment Selection: Detailed tumor profiling enables the selection of therapies that specifically target the most critical pathways driving tumor growth.
- Improved Side Effect Management: By understanding a patient’s broader medical history and current status, clinicians can adjust doses and regimens to reduce nerve-wracking side effects.
- Enhanced Response Rates: Tailoring treatment increases the likelihood of achieving a cytotoxic response, which may be essential for shrinking aggressive tumors.
This personalized approach, which deploys both traditional and innovative diagnostic strategies, is a key piece in managing later-line CRC treatments successfully. Patients are more likely to experience not only enhanced survival benefits but also an improved quality of life, which is an ultimate goal of any therapeutic strategy.
Future Perspectives: Steering Through Emerging Therapies and Technologies
The treatment of late-stage CRC is continually evolving. Emerging therapies and novel diagnostic tools are steadily adding to clinicians’ armamentarium. The integration of artificial intelligence (AI) in analyzing molecular data, for instance, promises to further refine patient profiling and therapeutic decision-making. As we get into the future, the hope is that emerging biomarkers and targeted agents will diminish the complicated pieces of late-line therapy choices.
Innovative Techniques on the Horizon
New studies are examining the use of artificial intelligence to help interpret complex molecular data more efficiently. Using AI-driven algorithms, physicians might soon be able to predict treatment responses based on subtle patterns in genetic and clinical data. Such innovations could shorten the decision-making cycle and help strike a balance between speed and accuracy—a valuable advancement when dealing with aggressive, later-line cancers.
Furthermore, emerging liquid biopsy platforms are aiming to lower costs and improve sensitivity. When these technologies become widely available and cost-effective, they could change the current standard of care. The benefits of faster turnaround times and a less intimidating procedure for patients may soon become the norm, transforming the overall patient experience in metastatic CRC.
Bridging the Gap Between Research and Routine Care
One of the ongoing challenges in cancer care is ensuring that the latest scientific breakthroughs reach the bedside quickly. Academic centers and pharmaceutical companies continue to work together to bring new therapies from the lab to real-world clinical settings. Collaboration between community-based practices and large research institutions plays a critical role here, ensuring that advances in personalized medicine and molecular diagnostics are accessible to all patient groups.
Efforts to conduct large, collaborative clinical trials will also help validate early promising results. Through these partnerships, hope is on the horizon for more streamlined and effective treatments that could substantially improve outcomes in metastatic CRC, even in its later stages.
Overcoming the Overwhelming: Practical Tips for Clinicians and Patients
Amidst all the innovative techniques and evolving treatment protocols, the real challenge remains providing clear guidance in the face of overwhelming treatment decisions. For both clinicians and patients, managing the nerve-racking process of selecting a later-line therapy involves more than just understanding molecular data—it involves balancing clinical judgment with the patient’s personal preferences and overall well-being.
Tips to Get Through the Toughest Bits in Treatment Planning
Here are some practical suggestions to help both clinicians and patients deal with the complicated pieces of later-line metastatic CRC care:
- Maintain open communication: Frequent discussions between the patient and the healthcare team can ease the pressure, making it easier to deal with unexpected twists and turns.
- Leverage a multidisciplinary team: Involving specialists from various fields ensures that all angles are considered—from molecular biologists to nurse practitioners specializing in symptom management.
- Regularly review clinical data: Constant evaluation of lab results, imaging studies, and patient symptoms helps keep the treatment plan up to date. Consider using both liquid and tumor biopsies when possible.
- Provide patient education: Empowering patients with knowledge about their disease and treatment options helps them feel more in control and less overwhelmed by nerve-wracking decisions.
- Consider clinical trial options: When standard therapies offer limited benefits, clinical trials can provide access to the latest therapies and contribute to ongoing research.
By following these simple yet effective strategies, clinicians can better steer through the tangled issues of later-line treatment, ensuring that patients receive individualized care while maintaining their quality of life.
Conclusion: Finding Your Path Through Later-Line Metastatic CRC Treatment
Later-line treatment for metastatic colorectal cancer is full of tricky parts that require a tailored, personalized approach to care. Through rapid molecular profiling, both liquid and tumor biopsies serve as essential tools in designing a treatment strategy that addresses a patient’s unique genetic and clinical landscape. While choices such as anti-EGFR rechallenge offer a potential for cytotoxic responses, they must be weighed against factors such as prior therapy exposure, molecular test results, and the patient’s overall health status.
The balance between speedy molecular diagnostics and maintaining cost-effectiveness remains one of the more overwhelming challenges. Yet, as emerging technologies continue to appear on the horizon, expectations for more efficient, affordable, and accurate testing methods are high.
Improving side effect management and ensuring robust, open communication are also super important factors in this journey. Every clinical decision—from deciding when to perform a liquid biopsy to selecting a suitable third-line regimen—plays a role in enhancing treatment outcomes and overall quality of life for patients facing this daunting diagnosis.
By embracing a multidisciplinary, patient-centered approach, and by staying abreast of the latest clinical data and emerging therapeutic options, clinicians and patients can make informed decisions that not only extend life but also preserve its quality. In the realm of metastatic CRC, every small twist and turn in the treatment pathway matters. It is through an understanding of each of these subtle details that we can truly learn to find our way through the tangled issues of late-stage treatment.
In closing, the future of metastatic colorectal cancer treatment lies in personalized medicine that leverages innovative diagnostics and targeted therapies. As we continue to dig into the fine points of cancer biology and treatment response, the hope remains that a fuller understanding of these tricky parts will lead to more precise, effective, and patient-friendly treatment options. For both clinicians and patients alike, making your way through these complicated pieces of care is an ongoing journey filled with challenges, but also with promise and progress.
Originally Post From https://www.targetedonc.com/view/navigating-metastatic-crc-treatment-options-in-later-lines
Read more about this topic at
Patient Navigation in Cancer Treatment: A Systematic …
A randomized trial of patient navigation with symptom …