Understanding Recurrent High-Grade NMIBC: A Closer Look
The management of recurrent high-grade non–muscle invasive bladder cancer (NMIBC) presents a series of tricky parts for both clinicians and patients. With varying treatment options, the decision-making process is loaded with issues that require both a scientific mindset and empathetic patient care. In this opinion editorial, we take a closer look at the recent findings from the CISTO study and examine the role of radical cystectomy compared to bladder-sparing therapy. We aim to provide an unbiased review that can help patients and clinical professionals figure a path through the confusing bits of treatment selection.
At its core, the CISTO study confronted one of the nerve-racking challenges in urology: how to best manage recurrent high-grade bladder cancer when the standard intravesical treatments like BCG have failed. The study was designed as a prospective observational cohort trial, engaging a large number of patients who were carefully balanced on various demographic and clinical characteristics. This rigorous approach allowed researchers to compare the benefits and drawbacks of undergoing radical cystectomy versus opting for bladder-sparing therapy.
What the CISTO Study Reveals About Treatment Approaches
The CISTO study, a well-funded investigation supported by the National Cancer Institute, has generated noteworthy insights. Patients who underwent radical cystectomy experienced improved recurrence-free survival (RFS) at 12 months compared to those who received bladder-sparing therapy. However, the decision to choose one treatment over the other is not as black and white as the numbers might suggest. Instead, each option carries its own set of advantages and complications that influence several aspects of patients’ lives.
The study reported that while radical cystectomy led to a significant improvement in recurrence-free survival—rising to about 96%—those in the bladder-sparing therapy arm saw a comparatively lower RFS rate. Interestingly, when it came to overall survival rates specific to bladder cancer and the 12-month physical functioning assessments, neither treatment showed a significant difference. This finding highlights the subtle, yet important, fine shades between aggressive surgical intervention and more conservative approaches.
Radical Cystectomy: Key Benefits and Concerns
Radical cystectomy, being a major surgery, understandably represents an intimidating prospect for many. Despite its nerve-racking nature, the study presents several arguments in its favor:
- Improved Recurrence-Free Survival: Patients who underwent the surgery experienced markedly better rates of remaining recurrence-free over a 12-month period.
- Better Global Health and Emotional Functioning: The study indicated that global health scores and emotional well-being were enhanced in patients who chose radical cystectomy compared to those on bladder-sparing regimens.
- Financial Considerations: Reports suggested that patients treated with radical cystectomy encountered fewer financial difficulties, a somewhat unexpected but critical factor in treatment choice.
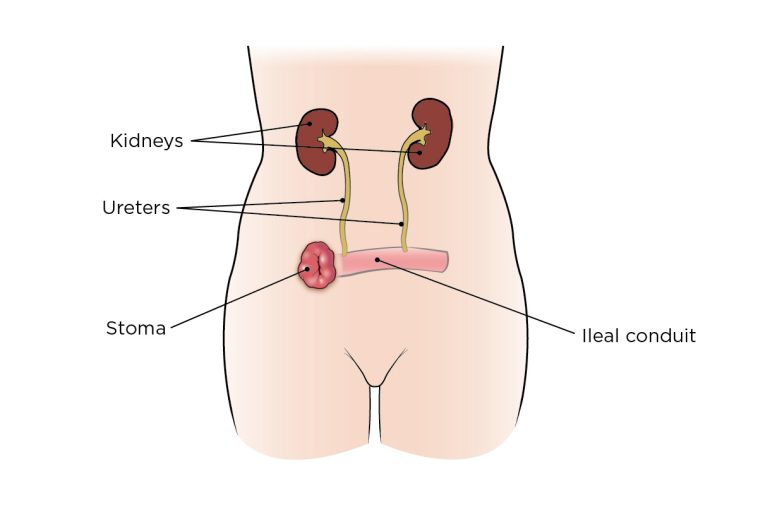
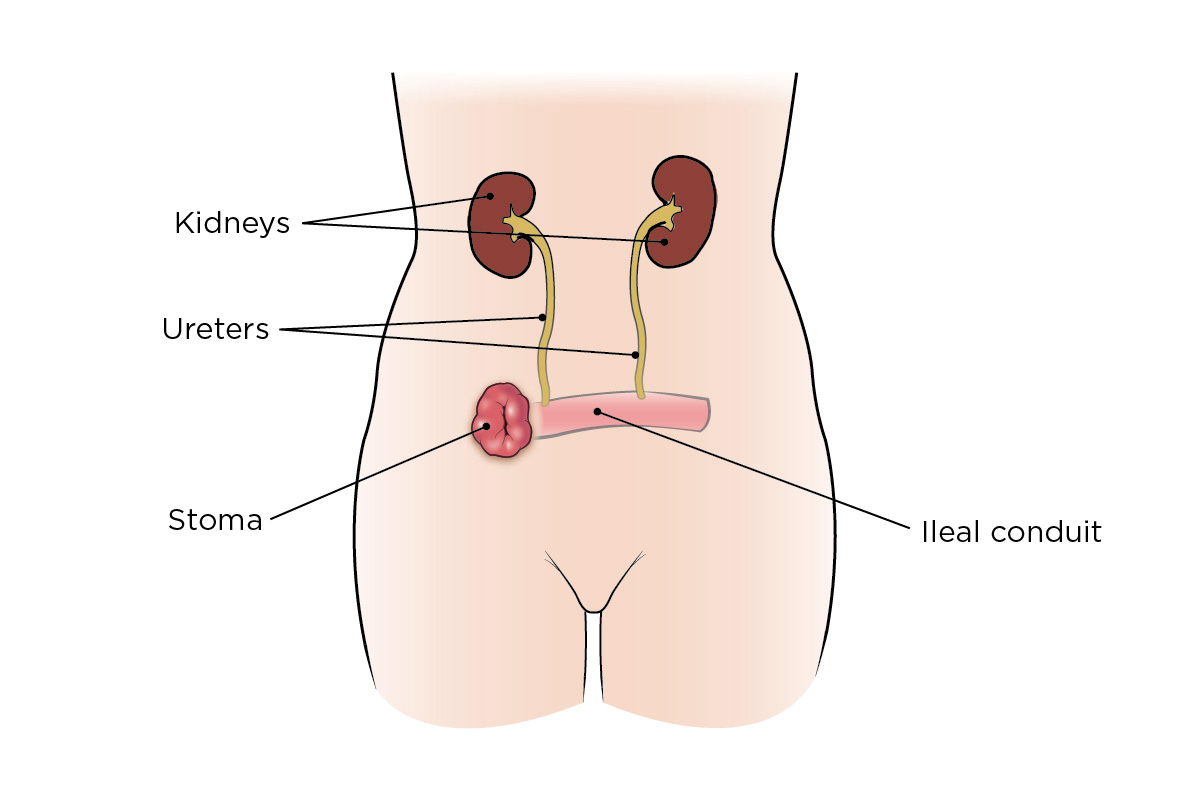
Despite these promising aspects, it is important to note the significant drawbacks associated with radical cystectomy. Patients reported worse outcomes in urinary, sexual, and bowel quality of life, highlighting the complicated pieces that must be seriously weighed when considering this aggressive treatment option. For many, the very thought of enduring such side effects can be overwhelming, and it calls for a careful dialogue between patients and their healthcare providers.
Bladder-Sparing Therapy: A Conservative Alternative
On the other side of the spectrum lies bladder-sparing therapy. This option is less invasive and can be a more acceptable route for patients averse to the challenges and potential hardships of major surgery. Bladder-sparing therapy is known to offer the following advantages:
- Less Intimidating Treatment Modality: Avoiding major surgery often means a quicker recovery period and fewer risks related to immediate postoperative complications.
- Better Progression-Free Survival: According to the study, bladder-sparing therapy demonstrated better progression-free survival. Although this benefit appears to stem largely from the pathologic upstaging noted in the radical cystectomy group, it remains a point of consideration for many clinicians.
- Preservation of Sexual, Urinary, and Bowel Function: While radical cystectomy compromises these aspects of quality of life, bladder-sparing approaches tend to protect them to a greater extent.
However, bladder-sparing therapy is not without its challenges. Its recurrence-free survival rates are lower than that offered by radical cystectomy, and the decision to use this modality after BCG failure leaves many patients full of problems regarding their long-term outlook. This dichotomy between quality of life and recurrence risk represents one of the tangled issues that continues to puzzle clinicians in the field.
Quality of Life Considerations: Balancing the Emotional and Physical
When discussing treatment for recurrent high-grade NMIBC, the fine points of quality of life should be given as much weight as the clinical outcomes. Patients are not only concerned about survival statistics but also about how treatment will affect their everyday lives—emotionally, physically, and even financially. The CISTO study provides important insights into these aspects:
Firstly, radical cystectomy was associated with improved global health and emotional functioning outcomes, despite its more intrusive nature. Patients undergoing the procedure reported feeling less depressed and anxious, which could be attributed to the reassurance provided by the reduced likelihood of recurrence. In essence, the peace of mind that comes from knowing the cancer is less likely to return can be a powerful motivator.
Conversely, those opting for bladder-sparing therapy, though spared the immediate hardships of major surgery, often faced ongoing stresses tied to the risk of recurrence and the cumulative uncertainties related to maintaining their bladder health over the long term. This trade-off is considered one of the slight differences that can tip the scale depending on an individual’s personal priorities and circumstances.
Investigating the Impact of Age and Comorbidities
The study also shed light on another layer of complexity: how age and other health conditions intersect with treatment choices. Interestingly, patients over 75 years of age demonstrated recovery trajectories that were comparable between the two treatment modalities. This finding suggests that even older patients, who are often thought to be more vulnerable to the rigors of surgery, might navigate the twists and turns of radical cystectomy without a significantly negative impact on their physical functioning.
Moreover, delving into the patient demographics reveals that those undergoing radical cystectomy were not only younger on average but also more likely to be partnered and had higher cancer severity at the time of treatment. This observation points to the idea that a strong personal support network, combined with a clearer clinical indication, may ease the journey through the intimidating realm of radical surgery. Meanwhile, patients who are single or carrying heavier comorbidities may favor a bladder-sparing approach to avoid further complicating their already full-of-problems healthcare profile.
Weighing the Pros and Cons: A Table of Treatment Outcomes
To help clarify the differences between the two treatment options, the following table summarizing the clinical outcomes and quality of life measures may be useful:
| Treatment Aspect | Radical Cystectomy | Bladder-Sparing Therapy |
|---|---|---|
| Recurrence-Free Survival (12 months) | Approximately 96% | Approximately 67% |
| Global Health and Emotional Functioning | Improved scores | Comparatively lower scores |
| Physical Functioning at 12 Months | Comparable recovery after initial decline | Comparable recovery overall |
| Urinary, Sexual, & Bowel Quality of Life | Worse outcomes | Better conservation of function |
| Progression-Free Survival | Lower, impacted by upstaging issues | Higher progression-free rates |
| Financial Toxicity | Lower financial strain reported | Higher financial strain |
This table not only organizes the benefits and trade-offs but also lays out the subtle details that need to be carefully considered before choosing the appropriate treatment approach. It is essential for patients and their care teams to review these factors thoroughly to make decisions that incorporate both the medical and personal dimensions of care.
Patient-Centric Decision Making in NMIBC Management
The path to choosing the right treatment for recurring bladder cancer is full of twists and turns, and it is heavily influenced by patient preferences, lifestyle factors, and support systems. In the wake of the CISTO study, it becomes increasingly clear that the decision-making process should not rely solely on clinical outcome statistics. Instead, it should also embrace the subjective experiences of patients as they weigh the pros and cons of each treatment option.
Many patients express concern over the nerve-racking idea of undergoing a major surgery. Even when the clinical data support the benefits of radical cystectomy for recurrence prevention, the personal costs—in terms of urinary, sexual, and bowel function—cannot be ignored. On the other hand, embracing bladder-sparing therapy may reduce the immediate physical burden but could lead to increased anxiety about the risk of cancer recurrence.
Engaging patients in the decision process is therefore super important. By openly discussing the little details such as anticipated recovery times, potential side effects, and emotional well-being, healthcare providers can help patients steer through the complicated pieces of modern bladder cancer care. It is beneficial to incorporate decision-support tools and patient education resources in this process, ensuring that every patient feels empowered when deciding their treatment trajectory.
Practical Considerations for Patients and Their Families
The journey through cancer treatment is often laden with both emotional challenges and tricky logistical issues. For patients and their families trying to get around these hurdles, having a clear understanding of both the benefits and disadvantages of each treatment can help in making an informed decision. Some practical steps include:
- Open Dialogue with Healthcare Providers: Ensure that all concerns, however small, are discussed in detail. This includes understanding the expected side effects and long-term implications on quality of life.
- Support Networks: Lean on family, friends, or support groups. Studies have shown that patients with a robust personal network tend to have better emotional outcomes, particularly after major procedures like radical cystectomy.
- Financial Planning: Arrange consultations with financial advisors who specialize in healthcare costs, as treatment expenses can vary significantly and financial stress can add an extra layer of difficulty.
- Rehabilitation and Follow-Up Care: Plan for postoperative care or regular monitoring after bladder-sparing therapy to promptly address any complications or recurring issues.
Healthcare providers and patients alike must work together to figure a path that best suits the unique circumstances of each individual. Aside from medical considerations, addressing these practical aspects can ease the nerve-racking process of managing recurrent high-grade NMIBC effectively.
Digging Into the Long-Term Implications of Treatment Choices
Beyond the immediate comparisons, the talk now shifts to the longer-term implications of choosing one treatment over another. The CISTO study remains ongoing, with further data expected to shed light on how these treatment strategies impact outcomes over several years. One of the most interesting future explorations involves understanding how the initial decision—radical cystectomy versus bladder-sparing therapy—affects long-term survival, quality of life, and overall patient satisfaction.
For instance, while radical cystectomy has demonstrated superiority in recurrence-free survival at the 12-month mark, the initial decline in physical functioning right after surgery is an aspect that many patients find intimidating. Fortunately, the study does provide a reassuring note: by the six-month mark, physical functioning appears to recover sufficiently, making the early decline a temporary setback rather than a lasting issue.
Similarly, bladder-sparing therapy’s advantage in progression-free survival must also be weighed carefully, especially as there is a significant concern regarding the impact of pathologic upstaging. Upstaging can lead to more complicated pieces in clinical management down the line—a detail that clinicians must discuss with their patients as part of long-term strategic planning.
Comparing Long-Term Outcomes: A Look at Clinical and Patient-Reported Data
While the short-term data offer significant insights, many clinicians stress the importance of integrating both clinical outcomes and patient-reported measures in the long-term evaluation. Some aspects warranting further scrutiny include:
- Overall Survival: Both treatment options have shown comparable bladder cancer-specific survival rates in the short term, indicating that neither method compromises long-term survival drastically.
- Patient-Reported Quality of Life: These subjective outcomes—covering emotional well-being, daily activity levels, and satisfaction with bodily functions—are critical in understanding how the treatment impacts life beyond just the clinical parameters.
- Secondary Complications: Ongoing monitoring for potential secondary complications such as urinary tract infections, sexual dysfunction, or bowel irregularities is necessary. Such issues can significantly affect the long-term recovery and lifestyle of patients.
Integrating these multi-faceted data points provides a more comprehensive picture of what patients might expect down the road. It also opens avenues for further research that considers both the measurable clinical outcomes and the more subtle details of patient quality of life. In this context, clinicians are better positioned to advise their patients on which path might be the most balanced and sustainable over the long haul.
Balancing Emotional Well-Being and Clinical Efficacy
It is no secret that a diagnosis of high-grade NMIBC often brings with it a mix of fear, uncertainty, and emotional strain. The findings from the CISTO study show that while radical cystectomy might be associated with some immediate physical setbacks—such as worse outcomes in urinary, sexual, and bowel quality of life—it could also provide emotional relief by reducing the risk of recurrence. This improved global health and emotional functioning is a critical point for many patients who value long-term peace of mind over short-term comfort.
On the flip side, patients who choose bladder-sparing therapy may experience a semblance of normalcy in their daily functions but might constantly worry about the possibility of the cancer re-emerging. This worry can be as intimidating as the physical side effects of surgery, and for some, it becomes a persistent mental load that affects their overall well-being.
Ultimately, the decision is a delicate balancing act between clinical efficacy and the everyday quality of life. It is essential for clinicians to take the time to understand each patient’s priorities and to discuss not only the medical facts but also the subtle details—the little twists—that matter most to the individual. By providing a well-rounded perspective and supporting patients emotionally during the decision-making process, healthcare providers can make a significant difference in the overall treatment journey.
The Role of Patient Advocacy and Education
In today’s healthcare environment, patient advocacy and education are key components of treatment planning. Organizations such as the Bladder Cancer Advocacy Network have played an important role in influencing the design of studies like CISTO. Their feedback clearly underscored that a randomized controlled trial comparing radical cystectomy and bladder-sparing therapy would be off-putting for many, with only a small percentage of patients comfortable with randomization.
As a result, the observational cohort design of the CISTO study was not only a scientific necessity but also a pragmatic decision aimed at respecting patient autonomy. Empowering patients with clear, unbiased information about both treatment options is super important to allay fears and facilitate a more informed, shared decision-making process.
For healthcare providers, this means going beyond merely sharing survival statistics. It involves taking the time to explain the fine points of each treatment—addressing concerns related to quality of life, recovery timeframes, and the potential for future complications. Such an approach can help patients feel more in control of what is otherwise an overwhelming decision.
Future Directions in NMIBC Treatment Research
As we continue to make sense of the findings from the CISTO study, one thing becomes abundantly clear: the landscape of NMIBC treatment is evolving. Future research will no doubt continue to poke around the long-term outcomes of both radical cystectomy and bladder-sparing therapy. Further insights are expected to address several questions that remain unresolved:
- How do the long-term survival rates compare beyond the 12-month window?
- What strategies can be adopted to mitigate the negative impact on urinary, sexual, and bowel functions post-cystectomy?
- Can innovative bladder-sparing techniques be developed to improve recurrence-free survival without compromising quality of life?
- How can personalized medicine approaches better predict which patients will benefit most from each treatment modality?
Such questions point to the necessity of ongoing studies that combine rigorous clinical endpoints with detailed, patient-driven feedback. Through sustained research efforts and better patient engagement, the chaotic bits of current treatment options can eventually be transformed into a structured roadmap that helps clinicians and patients alike figure a path to successful, individualized management of high-grade NMIBC.
Innovations in Surgical Technology and Patient Monitoring
One of the promising avenues for future exploration is the role of next-generation imaging and minimally invasive surgical techniques in the treatment of NMIBC. Innovations in these areas could potentially address some of the complicated pieces associated with radical cystectomy, such as the recovery timeline and the severity of postoperative complications.
For example, advances in robotic surgery and improved imaging protocols might help in minimizing the collateral damage that often leads to declines in urinary and sexual function. Combining these technological breakthroughs with comprehensive patient monitoring will not only refine the surgical process but also pave the way for more targeted bladder-sparing therapies.
Furthermore, emerging biomarkers and genomic testing could play a key role in identifying those patients who are more likely to experience recurrence irrespective of the initial treatment. By tailoring treatment plans to individual genetic profiles, clinicians may eventually overcome some of the hidden complexities that currently challenge the management of recurrent high-grade NMIBC.
Final Thoughts: Steering Through the Decision Maze
The journey through recurrent high-grade NMIBC treatment is undeniably complicated—a maze full of tangled issues and nerve-racking prospects. The CISTO study, with its comprehensive analysis of radical cystectomy versus bladder-sparing therapy, offers a wealth of insights that can help both patients and clinicians figure a path through these challenging decisions.
While radical cystectomy appears to offer a clear advantage in terms of recurrence-free survival, it comes with its own set of trade-offs that can adversely affect a patient’s quality of life. Bladder-sparing therapy, although less invasive and protective of certain bodily functions, may leave patients facing the ongoing anxiety of cancer recurrence.
The decision, therefore, must be made in a manner that carefully balances these factors. It involves not just reviewing the clinical outcomes, but also taking into account the subtle details of each patient’s lifestyle, emotional resilience, and personal priorities. By engaging in open, thoughtful discussions and utilizing patient-driven data, clinicians can support their patients in making a choice that feels right both medically and personally.
As the field continues to innovate, with ongoing studies and technological advancements, there is hope that the current challenges will gradually be replaced by more tailored and effective treatment strategies. In the meantime, it is super important for everyone involved to stay informed, ask questions, and work collaboratively in order to achieve the best possible outcomes for recurrent high-grade NMIBC.
Key Takeaways for Patients and Healthcare Providers
To summarize the discussion, here are some key points that both patients and medical professionals should keep in mind:
- Recurrence-Free Survival: Radical cystectomy demonstrates superior short-term recurrence-free survival, which is a critical consideration for many.
- Quality of Life Impact: The risks of worse urinary, sexual, and bowel function after radical cystectomy must be balanced against its benefits.
- Patient-Centric Decision Making: Treatment choices should be personalized, considering the patient’s age, support system, and personal preferences.
- Future Research Directions: Ongoing studies are expected to further clarify long-term outcomes, helping refine treatment recommendations.
- Technological and Innovative Advances: Emerging tools such as next-generation imaging, robotic surgery, and genomic profiling offer promise for more precise treatment planning.
In this evolving field, it remains critical that both clinicians and patients maintain a proactive approach to education and decision making. Whether choosing the more aggressive surgical route of radical cystectomy or the less invasive bladder-sparing therapy, understanding the tricky parts and hidden complexities of each option will ultimately lead to better outcomes and improved quality of life for those living with recurrent high-grade NMIBC.
Conclusion: Charting a Path Forward
The treatment of recurrent high-grade NMIBC is one of those medical areas where the science is robust but the decisions remain deeply personal. The CISTO study has provided valuable insights that illuminate both the benefits and limitations of radical cystectomy and bladder-sparing therapy. For patients, knowing the subtle distinctions between these approaches—ranging from recurrence-free survival rates to quality-of-life impacts—is key to making an informed choice that aligns with their values and lifestyle.
In our opinion, the future of NMIBC treatment lies in a balanced, patient-centric approach that respects the emotional, financial, and physical realities of each individual. While radical cystectomy may continue to play a key role in curbing cancer recurrence, its associated side effects necessitate thorough counseling. Meanwhile, bladder-sparing therapy, with its inherent advantages in preserving bodily function, must be accompanied by vigilant monitoring and robust patient support networks.
Ultimately, as we continue to sort out the many details in this ever-evolving field, it becomes clear that no single treatment pathway fits all patients. Instead, the decision-making process must steer through both the clinical data and the lived experiences of those affected. Whether you are a patient grappling with fear and uncertainty or a healthcare provider aiming to deliver the best care, taking a closer look at all the factors involved can help ensure that the path you choose is one that leads to not only longer survival but also a more fulfilling quality of life.
As ongoing research and advancements enrich our understanding of NMIBC management, we remain hopeful that future studies will further unravel the tangled issues surrounding treatment decisions. In the meantime, adopting a balanced, well-informed, and compassionate approach will help both patients and providers navigate this challenging terrain with confidence.
Practical Next Steps for Readers
If you or a loved one is faced with the decision between radical cystectomy and bladder-sparing therapy, consider these practical next steps to make an informed, collaborative decision:
- Schedule a Detailed Consultation: Engage deeply with your healthcare provider to understand both statistical outcomes and the expected day-to-day implications of each treatment option.
- Gather Second Opinions: Sometimes, hearing different perspectives from specialists can help untangle the twisted issues and provide further clarification.
- Connect with Support Groups: Patient advocacy groups and online forums can be invaluable in offering real-world experiences and advice.
- Review the Latest Research: Stay updated on ongoing studies like the CISTO trial, as emerging data may refine treatment strategies in the near future.
- Consider Personal Priorities: Reflect on what matters most to you—be it longevity, quality of life, or the balance between the two—and let that guide your decision-making process.
By combining clinical insights with patient experiences and leveraging new technological tools, we can make strides in demystifying the decision-making process associated with recurrent high-grade NMIBC. While the road ahead may still be loaded with issues, a proactive and informed approach can transform even the most intimidating treatment options into a journey marked by hope and perseverance.
In conclusion, whether you decide to take the wheel by opting for radical cystectomy or choose the bladder-sparing path, know that your choice reflects a deeply personal strategy to combat a challenging disease. Medical science continues to evolve, and with each new study and every innovative breakthrough, we get closer to an era where every patient’s treatment plan is as unique and carefully considered as their own life story.
Originally Post From https://www.urologytimes.com/view/cisto-radical-cystectomy-has-key-role-in-recurrent-high-grade-nmibc
Read more about this topic at
Fear of recurrence, breast-conserving surgery, and the …
Collaborative Review of Risk Benefit Trade-offs Between …