Immune Cells and a New Frontier in Acute Myeloid Leukemia Treatment
The evolving landscape of cancer therapy is no stranger to twists and turns. In the realm of cancer research, few diseases have been as intimidating and stubborn as acute myeloid leukemia (AML). Recent findings from a groundbreaking study conducted by Indiana University School of Medicine researchers are capturing attention. Their discovery of a previously unrecognized immune cell that may influence treatment outcomes in patients with AML prompts us to reexamine our approach to battling this aggressive blood cancer.
The Emergence of a Unique Immune Cell in AML
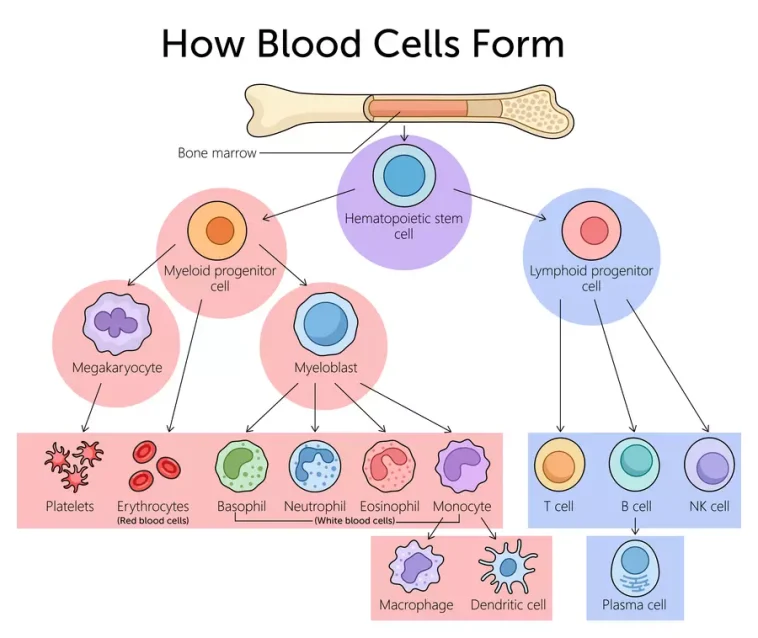
Acute myeloid leukemia, a cancer that begins in the bone marrow, continues to be a major challenge in modern medicine. Recognized as the sixth-leading cause of cancer-related death in adults, AML’s resistance to standard treatments and its tendency to relapse make it a formidable adversary. The recent study suggests that a unique type of regulatory T cell, which has often flown under the radar, plays a decisive role in undermining the body’s natural ability to fight off leukemia. This tiny cell type – hidden amid the complex bits of our immune system – may act as a shield, protecting malignant cells and helping them to survive current treatment regimens.
Why a Deeper Look at Immune Cells Matters
The discovery forces us to poke around the bone marrow’s hidden complexities in a new light. Researchers uncovered that these regulatory T cells, inherently designed to support the immune system, can turn against the body’s best interests when they accumulate in the bone marrow. Instead of performing their usual role of keeping other immune cells in check, these cells block cancer-fighting immune cells from engaging effectively with leukemia cells.
This finding is not only eye-opening—it is a reminder of how the immune system’s subtle details can have far-reaching impacts when the tiniest piece of the puzzle shifts its function. For patients who have long suffered from the overwhelming and nerve-racking nature of AML treatments, a strategy that avoids the tricky parts of treatment resistance is nothing short of a breakthrough.
Rewriting the Treatment Playbook: Targeted Antibody Therapy
One of the most promising outcomes of the study is the development of a new targeted antibody therapy. By focusing on the elimination of these misguided regulatory T cells, this innovative approach aims to lift the protective barrier that AML cells have long enjoyed. The therapy essentially reactivates the immune system’s natural ability to find its way through cancerous tissue, significantly improving survival in preclinical models.
In a field where progress has stalled for over three decades, the potential for a treatment option that is less toxic and more effective is super important. The proposed therapy could mark a pivotal shift in our strategy, countering the leukemia-protecting cells and enabling a more robust immune response. This development offers fresh hope to patients who have often found themselves caught in a cycle of relapse and limited treatment options.
Understanding the Immune System’s Role in AML
When we get into the fine points of the immune system’s operation in the context of cancers like AML, we begin to appreciate the minute details that can make or break a treatment plan. The discovery of this unique cell type highlights several key issues:
- The Hidden Complexity of Immune Responses: Despite being part of a system designed to protect, under certain circumstances, immune cells can become a double-edged sword.
- The Role of the Bone Marrow Microenvironment: The interaction between immune cells and cancer cells in the bone marrow is full of problems that require innovative thinking and strategies to overcome.
- Resistance to Conventional Therapies: Many existing treatments are not designed to address the tendency of these harmful cells to shield leukemia, contributing to treatment resistance.
These points underscore the necessity of making our way through the tangled issues of cancer immunotherapy. The immune system is not a monolithic entity; its subtle parts often hold the key to understanding why some therapies fail while others succeed.
The Broader Context: AML and the Current Treatment Landscape
AML is notorious for its intimidating treatment challenges and the nerve-racking side effects associated with traditional chemotherapy. Over the decades, clinicians have often been left with few options that offer a truly long-lasting remission. The standard treatment regimes, limited by their heavy toxicities and short-lived effects, demand a fresh perspective on combining immunotherapy with conventional methods.
Current treatment modalities for AML have largely remained unchanged, a fact that has sparked much debate among oncologists. New therapies must be designed not only to wipe out cancer cells but also to manage the hidden complexities introduced by the immune system’s own regulatory mechanisms. In this sense, the emergence of targeted antibody therapy represents a super important shift—one where the focus is on fine-tuning the immune response rather than simply bombarding cells with chemotherapy.
The Importance of Redefining Therapeutic Approaches
There are several reasons why this evolution in treatment is essential:
- Reduced Toxicity: The new strategy focuses on removing only the problematic T cells, potentially reducing the severe side effects often observed with traditional chemotherapy and high-dose treatments.
- Enhanced Immune Response: By removing the roadblocks preventing immune cells from attacking leukemia, the body’s own defenses are reactivated, meaning the treatment works with the body rather than against it.
- Prevention of Relapse: Targeting cells that promote resistance may help in developing more durable responses, lowering the risk of the disease returning after remission.
This rearticulation of protocols is a subtle reminder that the future of cancer treatment lies in our ability to find our way through the maze of immune interactions in the body. By ensuring that new treatments respect the natural architecture of the immune system, we make strides toward less toxic and more tailored interventions.
Breaking Down the Scientific Findings
The detailed study published in Nature Communications provides an in-depth look at how the immune system’s overlooked regulatory cells contribute to AML’s aggressive behavior. Researchers from multiple institutions, including experts from the Medical University of South Carolina and Indiana University School of Medicine, used preclinical models and human cell studies to draw their conclusions. Key findings from the study include:
| Key Discovery | Implication |
|---|---|
| Identification of a Unique Regulatory T Cell | Highlights how certain cells in the bone marrow hinder the immune system’s natural defense against leukemia. |
| Development of Targeted Antibody Therapy | Provides a focused strategy on removing harmful cells, potentially reducing treatment resistance. |
| Improved Survival in Preclinical Studies | Indicates the promising potential of this therapy in extending patient survival and lowering relapse rates. |
Every point in the table above signifies the importance of considering each slight difference in the immune system’s operation. The study draws attention not just to the discovery but also to the broader application of these insights in forming better, more effective therapies for AML patients.
Critical Analysis: Benefits and Limitations
The strengths of this approach are clear. By targeting the specific cells that support cancer growth, the therapy has the promise to reduce the toxicity often associated with broader treatments. However, like every strategy in medicine, there are some challenges hidden in the fine details:
- Preclinical to Clinical Transition: The promising results in mouse models and human cell studies need to be carefully translated into clinical trials. The journey from bench to bedside is often riddled with unexpected twists and turns.
- Potential Side Effects: While the therapy is designed to minimize collateral damage, precise modulation of the immune system must be managed meticulously to avoid unintended consequences.
- Patient Variability: AML is not a uniform disease. The effectiveness of the new strategy might vary depending on the individual patient’s immune profile and genetic background.
These points underscore the notion that even the most promising treatments must be scrutinized and refined through additional research. It is critical to work through the tangled issues and plan future studies that address every small distinction that could impact patient outcomes.
Shifting Perspectives: The Future of Cancer Immunotherapy
The study offers a glimpse into the future of cancer immunotherapy—a future where treatments are not only more precise but also more attuned to the body’s inherent defense mechanisms. For decades, AML treatment has been a rocky journey with nerve-racking setbacks. This new approach promises a smoother road ahead by integrating modern advances in antibody technology and deep biological insight.
By taking a closer look at the interplay between immune cells and malignant cells, researchers are working to figure a path that can ultimately lead to more effective and less invasive solutions. The targeted antibody therapy is more than just a new drug candidate; it embodies a philosophy that honors the intricate balance of the human immune response. This philosophy is gradually steering the field of oncology into an era where immunotherapy could become the cornerstone of treatment strategies for multiple types of cancers.
Implications for Clinical Practice
For healthcare professionals, this emerging data translates to an increased need to reexamine current treatment protocols in oncology and hematology. While the new immune cell discovery is still in the research phase, it offers several important implications for clinical practice:
- Personalized Medicine: Therapies that account for the subtle details and individual patient variations will likely become the norm. Doctors may soon have more tools to tailor treatments based on the patient’s unique immune profile.
- Adaptive Treatment Strategies: The ability to adjust immunotherapy according to dynamic factors in the tumor microenvironment could lower the rates of relapse and improve long-term remission.
- New Drug Development: Pharmaceutical research is expected to invest more in customizing antibody therapies that intervene in the specific immune pathways involved in cancers like AML.
As clinical settings begin to integrate these innovations, the dialogue between bench research and patient care becomes more critical than ever. It is essential that clinicians stay informed about the trial progress and remain open to adapting their treatment repertoire in line with emerging evidence.
Real-World Reflections: Patient Perspectives and Quality of Life
While scientific breakthroughs fuel hype in academic circles, it is the daily experiences of patients that ultimately validate the success of any new treatment. For those living with AML, the promise of a therapy that minimizes side effects and drastically improves survival prospects is a beacon of hope in otherwise intimidating circumstances.
Patients have long suffered from treatments that are both toxic and overwhelming. The reality of AML treatment is filled with nerve-racking procedures, constant monitoring, and an endless battle with relapse. The emerging targeted antibody therapy offers more than just clinical benefits—it promises a better quality of life by reducing the therapy-related burdens most patients have come to dread. For instance, fewer side effects could mean:
- Less time spending in hospitals and more time at home.
- Improved daily functioning and a return to a semblance of normalcy.
- Reduced anxiety over long-term health consequences.
By focusing on enhancing the immune system without overwhelming the body with toxic treatments, researchers are taking meaningful steps to ensure that patient comfort is not sacrificed at the altar of aggressive treatment. In this way, advancements in research are closely linked to improvements in everyday patient care, underscoring that the ultimate goal of medical innovation is to directly benefit those in need.
Community Impact and Advocacy
The news of this breakthrough has also spurred discussion among advocacy groups and patient communities. Many stakeholders are calling for increased funding and more research attention to AML, a disease that remains a major killer despite decades of effort. The broader community impact can be seen in the following areas:
- Raising Awareness: As more patients and families learn about the potential for improved outcomes, there is significant momentum behind advocacy for expanded research funding from governmental and non-governmental sources.
- Enhanced Clinical Trials: Patient interest in participating in clinical studies could drive faster recruitment and more robust data, expediting the timeline for translating laboratory findings into everyday treatments.
- Policy Shifts: Legislative and regulatory bodies might be persuaded to support innovative research avenues that promise to redefine standard care, ensuring that breakthroughs are not stalled by bureaucratic hurdles.
This dynamic interplay between scientific discovery, patient advocacy, and policy change illustrates that progress in healthcare is rarely confined to isolated labs. As research findings – such as the potential of targeted antibody therapy – begin to inform better treatment protocols, they also inspire collective action that can shape the future of cancer care on a broader scale.
The Road Ahead: Challenges and Opportunities in Clinical Translation
While the promise of new immunotherapy strategies is evident, the journey toward widespread clinical adoption is filled with tricky parts and confusing bits that require careful navigation. The task of taking a promising lab discovery and turning it into a life-saving treatment involves multiple stages:
- Clinical Trials: The preliminary results, though promising, must be rigorously tested in extensive clinical trials. This phase is both exciting and nerve-racking, as it will confirm whether the benefits observed in controlled settings translate to real-world patient care.
- Regulatory Approval: Even after successful trials, securing regulatory approval is a process full of tangled issues. Each data point, side effect, and outcome must be reviewed meticulously to ensure patient safety.
- Manufacturing and Distribution: Once approved, ensuring that the therapy can be produced, distributed, and administered efficiently remains a logistical and economic challenge.
Each step along this path is critical and requires robust support from multiple stakeholders. The collaboration between academic institutions, government agencies, and the pharmaceutical industry is key to fostering an environment where new treatments can flourish. The challenges may be intimidating, but the potential benefits are far too significant not to push forward with determined resilience.
Strategic Collaborations and Funding
The study itself was supported by funding from the National Institutes of Health, a testament to the value of investing in innovative research. As we step into a future where targeted therapies might become the norm, several strategies can help overcome the nerve-racking obstacles that lie ahead:
- Strengthening Public-Private Partnerships: Collaboration between large pharmaceutical companies and academic research centers can accelerate drug development by pooling resources and expertise.
- Increasing Transparency: Open communication of research progress and trial data fosters trust among patients, clinicians, and regulators alike.
- Fostering Global Research Networks: Bringing together experts from various fields and geographical locations can help smooth out the complicated pieces that are inherent in the clinical translation process.
These measures not only facilitate the current development of targeted antibody therapies for AML but also pave the way for broader applications in treating other cancers where the immune system is on edge. The future of cancer treatment hinges on our ability to figure a path through these obstacles in a way that supports innovation and patient safety simultaneously.
Conclusion: A Cautiously Optimistic Outlook
In the ever-evolving fight against acute myeloid leukemia, the discovery of a unique immune cell that plays a critical role in cancer resistance marks an essential milestone. What was once seen as just one more twist in the already tangled issues of immune regulation has now emerged as a promising target for novel therapies. The new targeted antibody therapy not only offers a less toxic alternative but also heralds a change in the way we approach immunotherapy for blood cancers.
Many of us in the medical field have spent years trying to figure a path through the nerve-racking maze of AML treatment. However, this breakthrough reminds us that progress—no matter how small the step—can accumulate into something transformative. By taking a closer look at the subtle parts that govern immune function, researchers are crafting strategies that could pave the way for more effective, personalized treatment protocols.
While challenges remain in translating these findings from preclinical studies to everyday clinical practice, the optimism is warranted. The collaborative nature of this research, combined with crucial support from institutions like the National Institutes of Health, sets the stage for what might be one of the next significant leaps forward in cancer treatment.
Moving forward, it will be essential for clinicians, researchers, and patient advocates to work side by side. There is a genuine need to steer through the complicated pieces of drug development and regulatory approval, address each small distinction within patient variability, and ultimately enhance the quality of life for individuals battling AML.
For patients and families facing an overwhelming diagnosis and daunting treatment regimens, these developments represent more than just promising figures in a research paper—they signal hope for a future where cancer care is more personalized, less toxic, and ultimately more effective. In this journey, every improved outcome is a victory, and every refined detail in therapy is a step closer to a world where the battle against acute myeloid leukemia can be fought and won with fewer side effects and better long-term survival rates.
By acknowledging both the progress made and the challenges that lie ahead, we come to appreciate that the future of cancer treatment relies not on a single discovery but rather on our collective ability to sift through the little details of biology, understand the nerve-racking components of disease, and work tirelessly to develop therapies that truly make a difference.
Key Takeaways for the Medical Community
In summary, the recent discoveries in AML research provide several lessons for the healthcare community:
- Innovative approaches to targeting problematic immune cells could revolutionize treatment protocols.
- Personalized therapies, which take account of individual immune profiles, may help reduce the severe side effects common in traditional treatments.
- Strong collaborations between research institutions, government agencies, and private companies are essential to successfully translate laboratory breakthroughs into clinical practice.
As healthcare professionals, keeping abreast of these developments is critical. It is super important that we engage in continuous dialogue, research, and clinical trials to ensure that the most effective strategies are brought to the forefront of cancer treatment. By doing so, we honor the immense potential of modern science and our shared commitment to providing care that not only treats the disease but also improves quality of life.
Looking Toward Tomorrow
The journey from groundbreaking research in the laboratory to improved survival rates in the clinic is full of the challenging bits we must carefully sort through. However, every twist and turn in this process reaffirms the resilience and ingenuity of the scientific community. With continued research that digs into the fine points of immune regulation, and with patient advocates driving forward the conversation about quality of life and treatment accessibility, the next chapter in AML treatment is promising indeed.
This study underscores one major reality: that the future of medicine lies in taking a closer look at the human body’s own intelligence. By refining our understanding of the immune system’s hidden complexities and continuously striving to improve its function, we not only enhance therapeutic outcomes but also pave the way for a more hopeful tomorrow for countless patients.
As we carry this momentum forward, it remains crucial to support innovative research while keeping patient well-being at the center of all advances. The lessons learned from tackling the nerve-racking challenges of AML should inspire broader application across other types of cancers and diseases loaded with issues that require creative, patient-centered solutions.
In conclusion, the discovery of a unique immune cell in AML provides a fresh lens through which we can re-examine our treatment strategies. With targeted antibody therapies on the horizon, and a renewed focus on personalized medicine, there is every reason to be cautiously optimistic about turning the tide against one of the most daunting blood cancers of our time.
Ultimately, embracing these new ideas with open minds and determined hearts will be the key to unlocking better outcomes for all. The path may be winding and full of confounding bits, but each step we take brings us closer to a future where effective, less toxic cancer therapies can transform lives.
Originally Post From https://www.newswise.com/articles/unique-immune-cell-linked-to-aggressive-leukemia-may-lead-to-improved-treatment-outcomes
Read more about this topic at
New “Smart” Immune Cells: A Breakthrough for Long- …
City of Hope Breakthrough Research Reveals an Immune …