Modern Approaches to Managing Metastatic Melanoma: An Opinion Editorial
In recent years, the treatment landscape for advanced or metastatic cutaneous melanoma has experienced tremendous evolution. With an increase in research and clinical trial data supporting the use of immunotherapy and novel cell therapies, clinicians are now better equipped to work through the tricky parts of patient care while providing treatment plans that are as individualized as the patients themselves. This opinion editorial will explore frontline immunotherapy treatment options, particularly focusing on combination immune checkpoint inhibitors and monotherapies. We will also discuss the challenges of balancing efficacy with toxicity, review the latest clinical evidence, and consider what the future may hold for patients battling advanced melanoma.
Working Through the Treatment Landscape of Advanced Melanoma
The journey of treating metastatic melanoma is far from straightforward. With an evolving array of clinical data and treatment strategies, making sense of the multitude of options can feel overwhelming for many clinicians. However, as recent panel discussions and expert peer exchanges have shown, there are a number of key strategies and treatment regimens that clinicians can consider as they work through the various treatment approaches.
Recent updates to guidelines by national organizations have placed a strong emphasis on immunotherapy as the primary treatment option for many patients. Experts are now critiquing and comparing the benefits of combination immune checkpoint inhibitors versus monotherapies. The primary goal across these discussions remains to achieve long-term, treatment-free survival while ensuring that therapy does not impose excessive toxicity. Given the advances over the past decade, it is now more important than ever to sort out the best approach for each patient while keeping their unique clinical factors in mind.
Digging Into the Fine Points of Frontline Immunotherapy
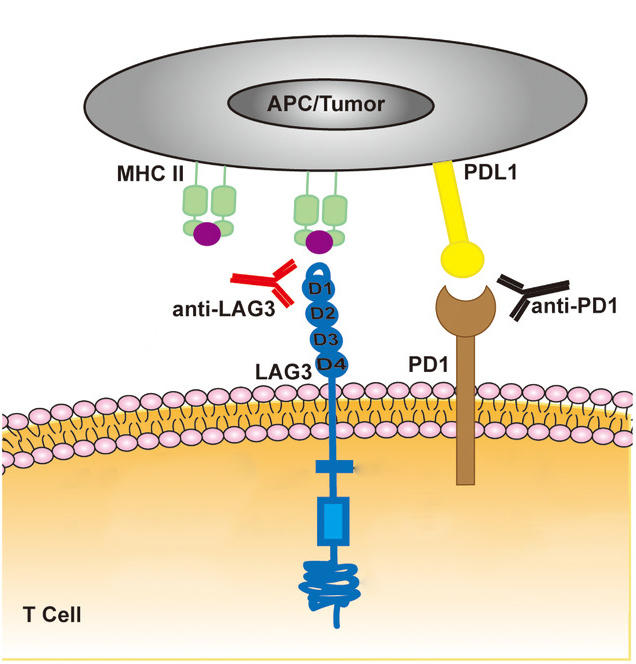
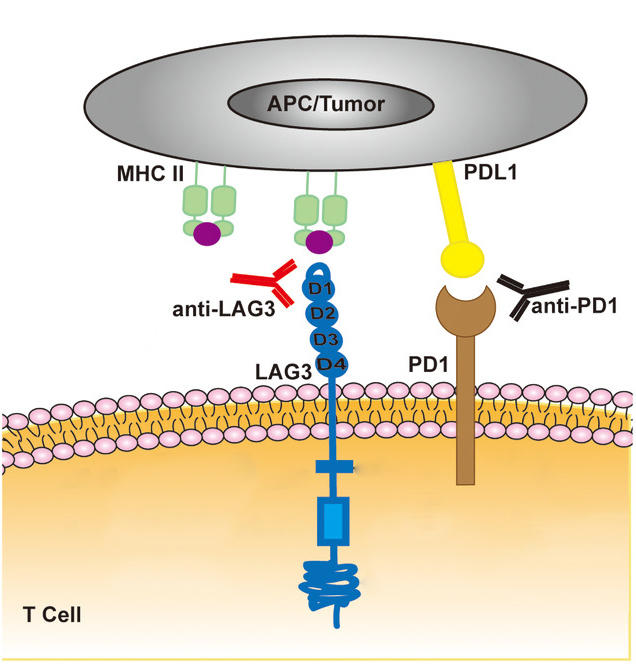
The term “frontline immunotherapy” encompasses several treatment regimens, each with its own subtle differences. Immunotherapy works by stimulating a patient’s own immune system to attack cancer cells, and over the last several years, clinicians have honed in on specific regimens that seem to offer the best balance of efficacy and manageable side effects.
Two primary combination regimens have emerged as frontrunners:
- Nivolumab plus Ipilimumab: This combination has been a mainstay in the treatment arena. It potently activates T-cells, though it also brings a higher risk of adverse effects. Given that the side effect profile can be intimidating, patient selection is incredibly important.
- Nivolumab plus Relatlimab: A more recent combination, which shows promise with a potentially more tolerable safety profile. This pairing is gaining support thanks to emerging data that points toward comparable survival outcomes while reducing some of the toxic risk seen with other combinations.
Clinicians must consider the hidden complexities of patient comorbidities and immune system status when determining whether a patient is best suited for a combination regimen or a monotherapy involving anti–PD-1 agents such as pembrolizumab or nivolumab. These agents, often recommended as Category 1 therapies in practice guidelines, have a history of strong clinical support while offering a more targeted approach with potentially fewer side effects.
Sifting Through the Tangled Issues of Monotherapies and Targeted Therapies
Apart from combination therapies, single-agent immunotherapy using PD-1 inhibitors remains a cornerstone treatment option for many clinicians. Monotherapies are typically considered when patient profiles suggest that the risks of combination therapies outweigh the benefits. Additionally, for patients with BRAF-mutated cancers, targeted therapies are also on the table as a preferred approach, further expanding treatment choices and adding layers of decision-making to the clinical process.
When assessing treatment options, clinicians are encouraged to consider factors such as:
- Patient age and overall performance status
- Genomic markers that might indicate a favorable response to immunotherapy
- The rate and extent of disease progression
- Potential interactions with other ongoing treatments
Though the clinical data are promising, many practitioners find themselves needing to balance the efficacy of these treatments with possible short- and long-term adverse effects. This tightrope walk requires a careful evaluation of both the benefits and the risks, and the decision-making process is often influenced by patient preference and tolerance levels.
Individualizing Treatment: Balancing Efficacy With Toxicity Concerns
There is no one-size-fits-all approach when it comes to treating metastatic melanoma. Each treatment regimen carries its own set of potential benefits and pitfalls, and the decision process is deeply personalized. Clinicians must weigh these options based on a patient’s specific clinical history, disease stage, and even personal treatment goals.
Assessing the Pros and Cons of Immunotherapy Regimens
When making a treatment choice, the following factors should be considered:
- Efficacy: Studies show that certain combinations can provide impressive overall survival benefits. However, head-to-head trials comparing these regimens remain limited, leaving some questions unanswered about the absolute superiority of one treatment over another.
- Toxicity: The adverse effects, which might range from immune-related adverse events to more severe systemic implications, often require constant vigilance. Some combinations, such as nivolumab with ipilimumab, are known to produce higher rates of these side effects, making them less appropriate for certain populations.
- Patient Quality of Life: Beyond clinical endpoints, the daily lived experience of patients is paramount. The goal is not just to extend life, but to ensure that patients can enjoy life during and after treatment. Achieving treatment-free long term survival is a primary objective that clinicians strive for.
Charting the balance between these factors requires more than an understanding of the science alone; it requires empathy and a high level of clinical judgment. Patients may be faced with decisions that are full of problems and might even seem off-putting, so continuous dialogue between physicians and patients is essential to ensure that treatment goals align with patient values and expectations.
Interpreting Clinical Trial Data: A Closer Look at Recent Studies
Recent updates from studies such as the RELATIVITY trial have brought to light many of the subtle details that guide current treatment strategies. While the data show that different immunotherapy combinations can achieve similar survival outcomes, the absence of head-to-head comparisons complicates the picture. Clinicians must therefore rely on indirect evidence and real-world experience to figure a path forward.
Key aspects of clinical data include:
| Parameter | Combination Regimen A (e.g., Nivolumab + Ipilimumab) | Combination Regimen B (e.g., Nivolumab + Relatlimab) |
|---|---|---|
| Response Rate | High | Comparable |
| Toxicity Profile | Higher adverse events | Moderate and potentially more tolerable |
| Suitability for Patient Profiles | More suitable for patients with robust performance status | May be chosen for patients in need of a gentler approach |
This table highlights the fine points that clinicians consider when comparing different treatment options. It is clear that while both regimens have the potential to deliver similar survival benefits, the choice can ultimately come down to balancing the fine details of efficacy and side effects.
Overcoming the Intimidating Twists and Turns of Clinical Decision-Making
The process of selecting the perfect treatment option is often fraught with challenges that can feel both overwhelming and nerve-racking to both clinicians and patients. The treatment journey, especially when dealing with a condition as aggressive as metastatic melanoma, involves managing the confusing bits of rapidly changing data and evolving clinical guidelines.
Weighing the Benefits and Risks: A Closer Look at Adverse Effects
For many patients, the possibility of adverse effects is one of the most intimidating considerations when starting immunotherapy. Some of the common adverse effects associated with combination immunotherapies include:
- Immune-mediated inflammation affecting the skin, liver, and gastrointestinal tract
- Fatigue and weakness
- Endocrine disorders, such as thyroid dysfunction
- Potentially serious events that require hospital admission
Many of these side effects are manageable, yet they require careful monitoring and often prompt intervention. Clinicians may sometimes need to step in quickly to adjust dosages or even switch treatment plans based on a patient’s response. This reactive process, while sometimes necessary, underscores the importance of personalized care plans that can be adjusted as newer data emerge and as patient circumstances change.
Strategies for Mitigating Risks in a Clinical Setting
Over the course of treatment, it is crucial that clinicians consider the following risk mitigation strategies:
- Regular Monitoring: Frequent check-ups and laboratory tests help in early detection of potential adverse effects. This proactive approach ensures that any complications can be addressed before they become severe.
- Patient Education: Empowering patients by explaining the possible side effects and what to expect can ease anxiety and promote timely reporting of any concerning symptoms.
- Multidisciplinary Coordination: Involving oncologists, dermatologists, endocrinologists, and primary care providers in a team-based approach aids in a more comprehensive management plan.
- Adaptive Treatment Plans: Being prepared to switch between treatment options if a certain regimen is not well-tolerated will ensure ongoing care without compromising treatment efficacy.
These strategies help clinicians to not only recognize the less obvious, twisting issues that can arise from long-term therapy but also to actively work through them with the patient, ensuring the best possible outcomes.
Real-World Clinical Observations and Practical Implications
While clinical trials provide statistically significant data and controlled environments, the real-world experience of administering these therapies can present a very different picture. Clinicians on the front lines are often responsible for adapting trial data to individual patient situations. As the research continues and patient outcomes are tracked in everyday clinical settings, practitioners are constantly learning from observed outcomes and making necessary adjustments in their treatment approaches.
Observations From Peer Exchanges and Multidisciplinary Conferences
Experts often come together in peer exchanges and interactive sessions to share their hands-on experiences and case studies. Many of these discussions reveal:
- The importance of patient selection in the success of combination immunotherapies
- Practicality of integrating genomic assessment into the standard of care
- Variations in treatment response that highlight the need for continued patient-specific adjustments
- Success stories where early intervention in adverse events led to better overall outcomes
These insights remind us that while statistical averages offer guidance, the fine shades of everyday clinical practice are what ultimately make a difference to each patient. The real-world application of research data is full of subtle details that require clinicians to maintain flexibility in their treatment planning.
Case Studies Reflecting Personalized Therapeutic Choices
Let’s consider a few illustrative examples:
- Case Study 1: A 55-year-old patient with advanced melanoma who initially received a combination of nivolumab and ipilimumab experienced significant adverse effects. With close monitoring and a shift toward a single-agent PD-1 inhibitor later, the patient’s quality of life improved markedly while still demonstrating a positive anti-tumor response.
- Case Study 2: Another patient with a history of autoimmune issues was initially not considered for combination therapy due to potential toxicity concerns. Instead, a targeted treatment plan using monotherapy and personalized genomic testing helped achieve the delicate balance between efficacy and safety.
- Case Study 3: A younger patient with robust performance status was able to manage the temporary side effects associated with combination therapy, leading to an extended treatment-free interval post-therapy. This case emphasizes the importance of patient-specific factors in deciding treatment regimens.
Each of these examples underscores the critical role that individualized treatment planning plays. Whether it is working through the tricky parts of regimen selection or managing side effects that can sometimes be confusing bits in the clinical picture, a tailored approach continues to prove essential in achieving optimal outcomes for patients.
Future Outlook: Essential Adaptive Strategies and Evolving Clinical Data
Looking ahead, the treatment landscape for metastatic melanoma shows promise for further refinement. Continuous research and more detailed clinical trials will likely offer clearer guidance on which treatment regimens are best suited for different patient populations.
Diving Into Upcoming Innovations and Treatments
Several developments are set to change the standard of care in the near future:
- Next-Generation Immunotherapies: Researchers are now exploring variants of established immunotherapy agents that may offer improved efficacy while reducing side effects. These advances include novel combinations and adjusted dosing regimens designed to provide better tolerability.
- Biomarker-Driven Decisions: As our understanding of the genomic and immune landscape in melanoma grows, the use of biomarkers to select appropriate treatment options is becoming more refined. This approach has the potential to transform treatment selection from a somewhat trial-and-error method into a predictable, individualized strategy.
- Integration of Cell Therapies: Besides immunotherapies, cell therapies such as CAR T-cell therapy are being evaluated for their role in advanced melanoma. Although still in the early stages, these therapies represent a shift toward more aggressive intervention strategies that could complement current treatment modalities.
These innovations highlight the need for clinicians to remain agile and informed. As more data become available, the treatment algorithms are expected to evolve, necessitating ongoing professional education and patient involvement in decision-making. The goal is to not only extend longevity but also maintain the highest possible quality of life for patients.
Strategies for Staying Updated in a Rapidly Changing Field
Clinicians and healthcare providers can take several steps to remain current in this ever-evolving field:
- Continuing Medical Education (CME): Participating in CME courses and conferences ensures that practitioners are up-to-date with the latest research and treatment strategies.
- Peer Exchanges and Collaborative Platforms: Taking part in multidisciplinary discussions with experts provides a platform for sharing experiences, challenges, and best practices.
- Subscribing to Trusted Journals and News Sources: Regularly reading publications and accessing reputable online resources can help clinicians obtain both the latest clinical data and real-world practical insights.
- Utilizing Decision-Support Tools: Integrating advanced clinical software and interactive algorithms can assist in fine-tuning treatment choices based on the most recent evidence.
These measures not only help in keeping up with clinical advances but also empower clinicians to tailor treatments specifically to the patient’s evolving needs. The willingness to adapt and update practices is one of the most valuable assets in maintaining excellence in patient care.
Working Through the Tricky Parts of Personalized Cancer Care
The paradigm shift toward personalized medicine in oncology represents one of the most significant changes in cancer care over the past decade. For advanced melanoma, this means moving away from a one-size-fits-all approach and embracing treatment regimens tailored to individual patient profiles.
Fine-Tuning Therapy Based on Patient-Specific Factors
Each case of metastatic melanoma is unique, making the role of the clinician as a guide and advisor more critical than ever. In forming a personalized treatment plan, clinicians need to consider a multitude of factors, including:
- Overall health and performance status
- Genetic markers and tumor mutation status
- Previous treatment responses or resistance patterns
- Patient preferences and lifestyle considerations
By taking these elements into account, clinicians can design treatment plans that not only target the cancer effectively but also allow patients to manage side effects and maintain a good quality of life. These individualized therapy decisions are the backbone of modern oncology practices, reflecting a move toward treatments that are both scientifically rigorous and personally empathetic.
Managing the Tough Bits: When Treatment Does Not Go as Planned
No treatment journey is without unexpected twists and turns. There are times when even the best-laid plans require modifications to better suit the patient’s changing condition or to address adverse effects as they occur. In these scenarios, clinicians must:
- Reassess the patient’s current clinical status through detailed examinations and imaging studies
- Consult with multidisciplinary teams to revise the treatment strategy
- Have honest and timely discussions with patients and their families regarding potential risks and benefits of continuing or changing therapies
- Document and review all changes to ensure that learning points are captured for future reference
This iterative approach to treatment planning not only enhances patient care in the moment but also contributes to the broader body of knowledge that will inform future clinical guidelines. By accepting that some outcomes may be unpredictable or on edge, clinicians are better prepared to provide the necessary support when treatment adjustments are needed.
Summing Up: A Comprehensive Path Forward for Immunotherapy in Melanoma
The landscape of frontline immunotherapy for advanced or metastatic cutaneous melanoma is ever-changing, with new research and innovative clinical strategies emerging regularly. The use of combination immune checkpoint inhibitors, along with carefully selected monotherapies, offers multiple pathways for extending survival and improving quality of life. Clinicians now have access to robust data, expert opinions, and real-world insights that help them work through tangled issues and figure a path among a growing array of treatment options.
Key takeaways from recent discussions include:
- The importance of individualized treatment approaches that consider both efficacy and toxicity.
- Strong support for combination therapies that, while more likely to produce side effects, can offer significant survival benefits for suitable patients.
- The evolving role of biomarkers and genomic testing in matching patients with the most appropriate therapy.
- A critical need for multidisciplinary collaboration – ensuring that treatment plans are continually reviewed, refined, and adapted as new evidence emerges.
Throughout this process, clinicians must remain both flexible and informed. The field is full of subtle details and small distinctions that can significantly impact patient outcomes. Whether it is by keeping abreast of the latest trial results or by integrating the hands-on experiences shared by peers, the focus remains on creating an environment where every decision is made with the patient’s best interest in mind.
Embracing Ongoing Education and Patient-Centered Care
It is clear that the future of advanced melanoma treatment will be defined by a commitment to continuous learning. Clinicians must remain vigilant and engaged in ongoing education, whether that comes in the form of attending conferences, participating in peer exchanges, or reading current research. By doing so, healthcare professionals ensure that their practices reflect the very latest in scientific discovery and practical experience.
At the same time, open and honest communication with patients is critical. When patients understand the reasoning behind different treatment choices and the possible side effects they may encounter, they are better positioned to participate in decision-making. This collaborative model not only respects patient autonomy but also maximizes the chance for improved outcomes over the long term.
Final Thoughts: Charting a Course Through the Evolving Treatment Maze
In conclusion, the treatment of metastatic melanoma is a journey filled with both promising opportunities and challenging twists and turns. The increased availability of immunotherapies, combined with targeted treatments and novel cell therapies, has revolutionized how clinicians work through the tricky parts of patient care. Future directions in research and clinical practice will likely bring even more refined approaches to tailoring treatments based on individual needs and emerging biomarkers.
For patients, this means that there is hope for treatments that do not simply prolong life, but also improve the quality of that life. For clinicians, it represents a call to remain open, reflective, and continually adaptive in their practices. As we move forward, the partnership between research progress, clinical judgment, and patient-centered care will remain at the heart of successful treatment strategies in metastatic melanoma.
Key Recommendations for Clinicians Moving Forward
To summarize the strategy for those keen on implementing the latest treatment approaches:
- Continuously update your knowledge through trusted medical education sources.
- Engage in multidisciplinary discussions to refine treatment decisions.
- Incorporate patient-specific details such as genetic markers and performance status into therapy selections.
- Develop risk mitigation strategies to address potential adverse effects early and proactively.
- Foster transparent communication with patients, ensuring they are partners in the therapeutic journey.
By following these recommendations, clinicians can better figure a path through the tangled issues of treatment selection and execution, leading to improved long-term outcomes and enhanced patient satisfaction.
Conclusion: A Commitment to Adaptation and Excellence in Care
The evolving field of immunotherapy for metastatic melanoma is a testament to the power of scientific inquiry and clinical perseverance. Despite the intimidating twists and turns that come with balancing treatment efficacy against toxicity, the pursuit of extending meaningful life for patients has never been more active or hopeful. As research continues to uncover new insights, it remains critical for healthcare professionals to remain engaged and adaptable, ensuring that each treatment plan is both scientifically rigorous and deeply personal.
Ultimately, our shared goal should be to not only treat the disease but also to support each patient’s quality of life. By embracing innovative therapies, applying real-world clinical data, and engaging in honest dialogue with patients, clinicians can chart a comprehensive and patient-centered course through the evolving treatment maze. This commitment to adaptation and excellence in care will ensure that for many years to come, patients with metastatic melanoma have access to therapies that are both effective and compassionate.
In this era of precision medicine, every new piece of evidence, every case study, and every patient story adds a small twist to the broader narrative of cancer care. Let us use each of those lessons as a stepping stone on our journey to not only cure, but to truly care.
Originally Post From https://www.onclive.com/view/frontline-immunotherapy-treatment-options-in-advanced-or-metastatic-cutaneous-melanoma
Read more about this topic at
New Approaches on Cancer Immunotherapy – PMC
Contemporary Approaches to Immunotherapy of Solid …