Chronic Subdural Hematoma: A Shifting Landscape in Neurosurgical Care
The management of chronic subdural hematoma (CSDH) has been a topic of heated discussion in the healthcare community for many years. With an annual incidence that ranges from 1.7 to 20.6 per 100,000 people—and climbing due to an aging global population and increasing use of anticoagulant therapies—the condition is at the heart of many debates among neurosurgeons and clinicians alike. In this opinion editorial, we take a closer look at the evolving nature of CSDH management, discuss the tricky parts of its pathogenesis, review the surgical and non-surgical options, and examine promising future interventions such as middle meningeal artery embolization (MMAE).
As an editor for an online healthcare journal, I have seen firsthand the impact of both innovative procedures and evolving research in transforming patient care. With the growing burden of CSDH, especially among the elderly, our approach to diagnosis and treatment requires a balanced perspective that considers both the potential benefits and the hidden complexities.
Aging Population and Antithrombotic Therapies: Driving the Rise of CSDH Incidence
One of the key factors behind the increasing incidence of chronic subdural hematoma is the elderly demographic. As life expectancy increases, the number of older adults—who are more likely to fall and sustain head injuries—continues to rise. This demographic shift is compounded by the widespread use of anticoagulants and antiplatelet medications in managing cardiovascular conditions, making minor traumas riskier and more likely to lead to CSDH formation.
When we take a closer look at the epidemiological data:
- The incidence among those over 80 years old can be as high as 127.1 per 100,000 individuals.
- Along with increased falls, the use of antithrombotic medications further complicates the clinical picture.
- By 2030, experts predict that CSDH might become the most frequent condition encountered in cranial surgery, possibly even surpassing brain tumors.
This evolving landscape makes it super important that we continue refining both our clinical tools and therapeutic techniques to properly manage the condition. In many ways, the increasing prevalence of CSDH has pushed the medical community to take a closer look at every stage of the treatment process—from diagnosis to post-operative care—so that we can better steer through these challenging cases.
Unraveling the Tricky Parts of CSDH Pathogenesis: Inflammation, Trauma, and Angiogenesis
Traditionally, the cause of chronic subdural hematoma was attributed to the rupture of bridging veins from head trauma. However, recent studies have emphasized that this explanation may only partially capture the true nature of the condition, especially in non-traumatic cases.
Today, research suggests that the development of CSDH is a tangled interplay of inflammatory processes, fibrinolytic dysregulation, and new blood vessel formation (angiogenesis). The injury to the dural border cell layer sets off a chain reaction that leads to release of key mediators like vascular endothelial growth factor (VEGF) and pro-inflammatory cytokines (for example IL-6 and IL-8). These substances are central to triggering the formation of membranes and causing recurrent microbleeds from fragile new vessels.
Here are some of the little details that underline the current understanding of CSDH pathogenesis:
- Inflammatory Cascade: The interplay of cytokines contributes to an ongoing self-perpetuating cycle that promotes hematoma enlargement.
- Fibrinolytic Imbalance: Changes in the balance between coagulation and fibrinolysis increase the likelihood of rebleeding.
- Neovascularization: The formation of fragile new vessels fuels further bleeding, complicating the natural history of the hematoma.
This blend of trauma-induced injury and the body’s own inflammatory response creates a condition loaded with issues that make managing CSDH particularly nerve-racking for clinicians. With each new study, we are forced to dig into these confusing bits of its biology to identify intervention points that might halt or reverse the disease process.
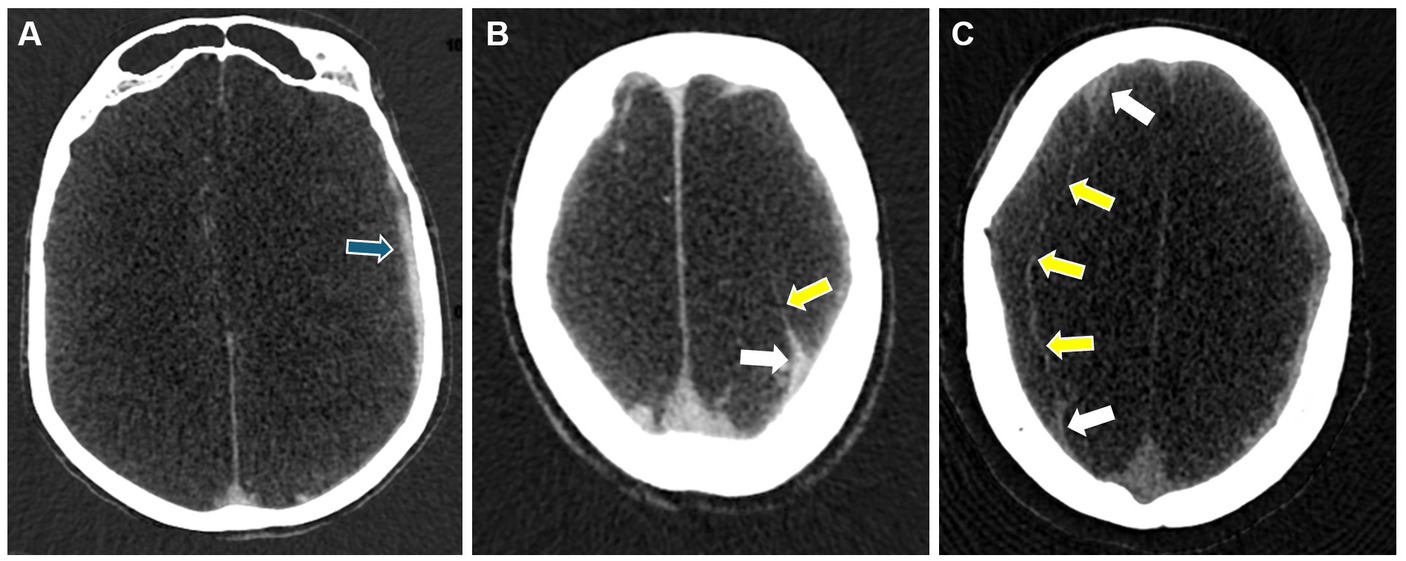
Advanced Imaging Techniques: Enhanced Visualization Amidst the Hidden Complexities
Accurate diagnosis is absolutely critical in the management of chronic subdural hematoma. While computed tomography (CT) remains the go-to imaging tool for a quick assessment, there are several challenges that call for a more nuanced approach. CT imaging, which typically shows a crescent-shaped collection of blood, can sometimes miss the finer details such as small or isodense hematomas, thereby complicating the diagnosis. Moreover, the internal architecture of the hematoma is often not fully appreciated on CT scans.
Magnetic resonance imaging (MRI) offers a more refined look, thanks to its superior soft-tissue resolution. With MRI, radiologists are better equipped to expose the septations and membrane structures that often serve as clues to the hematoma’s maturity and its propensity to recur. Modern MRI techniques, such as diffusion-weighted imaging, have added another layer of detail—helping to figure a path through the labyrinth of CSDH’s internal structure.
The benefits of advanced imaging include:
| Imaging Modality | Advantages | Limitations |
|---|---|---|
| CT Scan |
|
|
| MRI |
|
|
While no single imaging modality can claim absolute perfection, the combination of CT for initial evaluation and MRI for detailed assessment represents one of the most effective strategies in modern clinical practice. This dual approach helps clinicians orient themselves in what can sometimes seem like a series of twists and turns when diagnosing CSDH.
Advances in Surgical Techniques: Weighing the Pros and Cons of Invasive Procedures
Surgery remains the most widely accepted option for treating symptomatic CSDH, particularly when there is significant mass effect causing neurological impairment. Yet, even in the realm of surgical interventions, there are many small distinctions in technique that can make a big difference in patient outcomes.
The primary surgical strategies include:
- Twist-Drill Craniostomy (TDC): A minimally invasive procedure that can often be performed at the bedside. However, TDC is associated with a somewhat higher risk of recurrence and the potential for cortical injury.
- Burr-Hole Craniostomy (BHC): The most popular method in use today. It boasts high efficacy and low morbidity, though recurrence can remain a lingering issue. Variations such as the type of irrigation fluid used or decisions about drain placement continue to spark debate.
- Craniotomy: Reserved for more complicated or recurrent hematomas which involve well-organized membranes. Although craniotomy offers the possibility of extensive membrane removal, it also carries higher risks in terms of complications and mortality.
- Endoscopic-Assisted Evacuation: This modern approach allows direct visualization and more complete removal of the membranes thought to contribute to recurrence. Despite its potential for reducing repeated interventions, it requires significant surgical expertise and may extend the operative time.
Below is a table that neatly summarizes the various surgical options, highlighting some of the key pros and cons associated with each method:
| Surgical Technique | Advantages | Challenges |
|---|---|---|
| Twist-Drill Craniostomy (TDC) |
|
|
| Burr-Hole Craniostomy (BHC) |
|
|
| Craniotomy |
|
|
| Endoscopic-Assisted Evacuation |
|
|
The choice of surgical technique ultimately depends on several factors including patient age, overall health, the nature of the hematoma, and the likelihood of recurrence. As with many areas in medicine, there is no one-size-fits-all approach—and it is the surgeon’s responsibility to figure a path that best fits the unique situation of each patient.
Innovative Middle Meningeal Artery Embolization: A New Frontier in Minimally Invasive Treatment
Perhaps one of the most captivating developments in the management of CSDH is the emergence of middle meningeal artery embolization (MMAE). This technique targets the neovascularization that causes persistent bleeding and hematoma recurrence by embolizing the middle meningeal artery. The idea behind MMAE is to cut off blood supply to the fragile membranes, thereby curbing the cycle of inflammation and recurrent microbleeds.
MMAE is increasingly being used either as a standalone treatment or as an adjunct to traditional surgical interventions—especially in high-risk patients who are on long-term anticoagulants or have experienced multiple recurrences. Several studies have indicated recurrence rates as low as 4.3% with MMAE, suggesting that it might offer a safer, less invasive alternative for many patients.
Below, we highlight some of the key benefits and current challenges faced by MMAE:
- Benefits:
- Minimally invasive with reduced recovery times
- Targets the core issue of neovascularization
- Can be combined with surgery for a multi-modal approach
- Challenges:
- Limited data on its effectiveness in acute symptom relief
- Requires specialized interventional expertise
- Long-term outcomes are still being studied
This technique represents a paradigm shift in the treatment of CSDH, offering clinicians another tool to manage a condition that has long been on edge due to its recurrent nature. With ongoing research and randomized controlled trials, we expect that the precise role of MMAE in managing CSDH will continue to become clearer in the coming years.
Pharmacological and Conservative Interventions: Exploring Alternative Routes to CSDH Management
Not every patient is an ideal candidate for surgery or invasive interventions. For those who are asymptomatic or categorized as high-risk, a conservative pharmacological approach may be the preferred strategy. A growing body of research is exploring non-surgical therapies that focus on modulating the body’s inflammatory response and angiogenic processes.
Some of the key pharmacological agents under investigation include:
- Atorvastatin: Known for its ability to reduce inflammation and promote vascular repair, it has shown promise in decreasing hematoma volume and preventing recurrence.
- Corticosteroids: These potent anti-inflammatory agents can help manage the post-injury inflammatory response, although their long-term use comes with a range of side effects.
- Tranexamic Acid (TXA): This antifibrinolytic drug may help reduce the risk of rebleeding by inhibiting the breakdown of blood clots, though more research is needed regarding its safety profile, especially among the elderly.
- ACE Inhibitors: While these agents have been studied for their possible influence on angiogenesis, the data remains conflicting regarding their role and efficacy in preventing CSDH recurrence.
- Herbal Medicine Agents: Early studies, such as those examining Goreisan, suggest that certain herbal formulations might help reduce recurrence, though comprehensive clinical evidence is yet to be gathered.
For patients and clinicians alike, the decision to steer away from surgery can be nerve-racking. Balancing the potential benefits of these pharmacological interventions against their side effects is a delicate process that involves careful assessment of each patient’s overall risk profile and the specific nature of their hematoma.
Future Directions: Finding Effective Strategies Amidst Complicated Pieces
There is no denying that chronic subdural hematoma remains a condition loaded with issues. Despite significant advancements in our understanding of its pathogenesis and treatment, we continue to face several challenging aspects that need to be addressed. The following key areas should shape future research and clinical protocols:
- Clarifying the Underlying Mechanisms: A deeper exploration of the inflammatory and angiogenic processes involved is necessary to reveal precisely where we might intervene with more targeted therapies.
- Standardizing Surgical Approaches: With various surgical techniques available, reaching a consensus on best practices and perioperative care protocols will be essential in reducing recurrence and avoiding complications.
- Expanding the Evidence Base for MMAE: Randomized controlled trials are critically needed to validate the effectiveness and long-term safety of middle meningeal artery embolization, both as a standalone therapy and as an adjunct to surgery.
- Optimizing Combination Therapies: Researchers are beginning to explore the synergistic effects of combining pharmacological agents (like statins with corticosteroids) alongside minimally invasive techniques. This multi-modal approach could provide a more comprehensive treatment strategy for patients at high risk of recurrence.
- Personalized Patient Management: Variation in individual patient factors, including age, comorbidities, and medication use, calls for a more personalized approach to treatment. Tailoring therapy to each patient’s unique situation is super important in achieving the best possible outcomes.
While many of these areas are still in the early stages of investigation, their potential to transform the management of CSDH is clear. The ultimate goal is to integrate mechanistic insights with practical clinical strategies that improve both short-term recovery and long-term patient well-being. As researchers and clinicians continue to poke around the subtle parts of this condition, their findings will undoubtedly lead to more effective and safer treatment protocols.
Balancing Innovation with Prudence: The Road Ahead in CSDH Management
The evolution of chronic subdural hematoma management is a striking example of how advances in science and technology can reshape clinical practice. Confronted with a condition that is both intricate and on edge, healthcare professionals have had to explore every possible angle—from imaging to pharmacology—to offer patients the best possible care.
It is worth noting that, despite the promise of novel techniques like MMAE and enhanced imaging strategies, surgical evacuation remains the bedrock of treatment for symptomatic CSDH. The surgeon’s ability to carefully figure a path through the myriad of treatment options is crucial. This decision-making process involves weighing the benefits of a minimally invasive approach against the potential for complications, and it often requires a delicate balance between ambition and caution.
The evolution of treatment strategies can be seen as a journey fraught with both progress and setbacks. Over the past two decades, breakthroughs have been somewhat limited—not because of a lack of clinical expertise or technological advancement, but because of the fundamental need to understand the tricky anatomy and physiology of CSDH. The interplay between inflammation, angiogenesis, and trauma presents a set of tangled issues that are not easily untangled.
From our vantage point in modern medicine, the future of CSDH treatment seems promising, yet it remains a field where more evidence is needed before sweeping changes can be embraced universally. Nonetheless, every incremental step—from advanced imaging to refined surgical techniques and pharmaceutical trials—brings us closer to a scenario where patients receive treatments that are both effective and tailored to their unique medical circumstances.
Expert Opinions and Community Perspectives: A Conversation on CSDH
The dialogue among neurosurgeons, radiologists, and pharmacologists regarding the optimal management of CSDH is as interesting as it is complex. Many experts have voiced that the integration of multidisciplinary approaches is key. They emphasize:
- The need to address both the head-on challenges of recurrence and the underlying small distinctions that define each patient’s condition.
- The importance of staying updated with the latest imaging techniques to ensure that every tiny bleed or membranous change is caught early.
- How combining innovative interventions like MMAE with traditional surgical options may offer the best chance of long-term success.
These discussions are not just academic—they have real-world implications for patient outcomes. Healthcare professionals are constantly refining their protocols, guided by emerging research that helps illuminate the previously murky aspects of CSDH pathogenesis and treatment. Future conferences, published studies, and clinical trials will no doubt continue to shape how we manage this condition on a daily basis.
In many ways, the success in managing CSDH is a testament to the power of collaboration. Neurosurgeons, radiologists, and pharmacologists are all working together, each contributing their unique insights to manage the unpredictable twists and turns of this condition. It is through this combined effort that we begin to picture a future where CSDH can be effectively managed with a combination of precise techniques, targeted therapies, and personalized patient care.
Conclusion: Embracing the Future of CSDH Management with Caution and Optimism
In conclusion, chronic subdural hematoma represents one of the most challenging neurosurgical conditions—especially as its incidence climbs amidst the backdrop of an aging population and widespread antithrombotic use. Its management is a journey through a maze of tricky parts, from the tangled issues of pathogenesis to the delicate decisions involved in surgical intervention. While traditional approaches like burr-hole craniostomy remain critical, the emergence of techniques like middle meningeal artery embolization provides a promising glimpse into the future.
Moreover, the advances in imaging and pharmacological research are opening new avenues for conservative management, particularly for those high-risk or asymptomatic patients who might otherwise face the nerve-racking prospect of surgery. By taking a balanced approach—one that includes a combination of advanced diagnostics, minimally invasive techniques, and personalized patient care—clinicians can work through the complicated pieces involved in CSDH management.
Looking ahead, more randomized trials and collaborative studies will be needed to validate these emerging strategies and integrate them into standard clinical practice. Until then, the treatment of chronic subdural hematoma remains both a cutting-edge and a carefully calibrated field, reflecting the ongoing commitment of the medical community to patient well-being, even amidst many challenging small distinctions.
For those of us in modern healthcare, it is clear that every advance—whether in imaging or in surgical technique—represents a crucial step forward in our endeavor to improve the quality of life for patients with CSDH. With continued innovation and thoughtful application of current knowledge, we can hope to transform what was once seen as an overwhelming medical challenge into a condition that is managed with precision and care.
In this time of rapid medical evolution, the conversation around chronic subdural hematoma is far from over. As research delves deeper into the subtle details of its pathology and treatment, we remain optimistic that a blend of traditional wisdom and innovative practice will lead the way to safer, more effective management options for all those affected by this condition.
Originally Post From https://www.news-medical.net/news/20251118/Advances-in-diagnosis-and-management-of-chronic-subdural-hematoma.aspx
Read more about this topic at
Hematoma Management
Innovative Treatment for Subdural Hematoma