Revolutionizing Diabetic Retinopathy Treatment with Continuous Delivery Systems
Diabetic retinopathy continues to be one of the most challenging eye conditions to manage. As the prevalence of diabetes increases, so does the number of individuals facing this potentially vision-threatening complication. Over the years, the treatment approach has mainly involved repeated eye injections that can be both intimidating and nerve-racking for patients. Today, however, a breakthrough treatment, Roche’s Susvimo, offers hope by providing a continuous drug delivery system that requires only one refill every nine months. In this editorial, we take a closer look at the new treatment approach, discuss the benefits and potential concerns, and examine how this innovative therapy might reshape diabetic retinopathy care.
Unlike traditional anti-VEGF injections that require monthly or bi-monthly visits, Susvimo represents a significant departure from the typical regimen. This sustained-release technology moves away from the conventional treatment model by offering extended intervals between treatments, thus reducing the frequency of clinic visits and providing an opportunity for improved patient adherence and overall quality of life.
Innovative Sustained Release Therapy for Diabetic Retinopathy
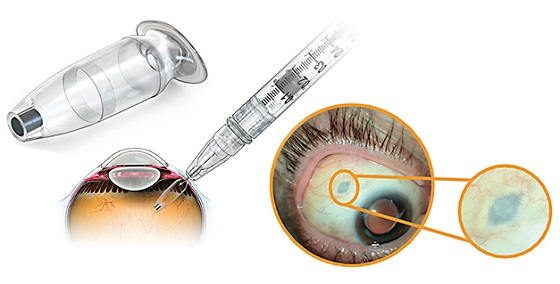
The emergence of continuous drug delivery for diabetic retinopathy is a topic that has stirred considerable excitement within the healthcare community. This innovative sustained release therapy leverages a unique drug-delivery implant designed to provide steady levels of ranibizumab over an extended period. For patients, this means fewer disruptions in their daily lives and less exposure to the tricky parts associated with frequent invasive procedures.
The continuous delivery system within Susvimo ensures that patients receive a steady dose of medication that helps maintain vision and possibly prevent further deterioration. Such an approach is seen as a key advancement because it addresses not only the treatment effectiveness but also the patient experience—a factor often loaded with issues when dealing with traditional multiple injection regimens.
Why Continuous Drug Delivery Is a Game-Changer
For many patients, the prospect of monthly eye injections can be both confusing and intimidating. With traditional treatments, there are many twists and turns, from scheduling consistent appointments to managing side effects and the overall stress associated with frequent treatments. The continuous drug delivery system aims to mitigate these challenges by reducing the treatment frequency. One refill every nine months offers a much-needed reprieve and enables patients to steer through their daily lives with reduced clinic visits.
Furthermore, the continuous therapy taps into a critical demand in modern medicine: treatments that put the patient first. Instead of a one-size-fits-all approach, continuous delivery is tailored for patients who have already responded to at least two anti-VEGF injections, ensuring that the treatment is both effective and safe. This patient-centric evolution in therapy could well represent the future of managing diabetic retinopathy.
Evaluating the Phase III Pavilion Trial Outcomes for Diabetic Retinopathy
Scientific studies serve as the cornerstone for advancing clinical practice, and the Phase III Pavilion trial has provided a treasure trove of data on Susvimo’s performance. In this extensive trial, 174 patients were carefully observed over a one-year period to assess the safety, efficacy, and long-term benefits of this novel treatment. The results painted a promising picture, with 80.1% of patients achieving at least a two-step improvement on the Diabetic Retinopathy Severity Scale (DRSS) compared to only 9% in the control group.
The trial design was straightforward yet meticulous, focusing on patients under monthly clinical observation. Two initial Susvimo injections were provided before the treatment group underwent the implant procedure at week four. This structured approach allowed clinicians to monitor the nitty-gritty of the treatment’s performance. The dramatic contrast in patient outcomes highlights the potential of continuous therapy to offer sustained vision benefits and a reduced need for supplemental treatment compared to traditional therapies.
Key Findings from the Pavilion Trial
- Sustained Improvement: The majority of treated subjects experienced significant improvements on the DRSS, demonstrating that continuous release of ranibizumab can positively affect the stability of diabetic retinopathy.
- Reduced Vision-Threatening Complications: The trial showed a stark decrease in the progression to vision-threatening complications such as center-involved diabetic macular edema, proliferative diabetic retinopathy, and anterior segment neovascularization. This reduction in risk is one of the standout benefits of using a continuous delivery system.
- Visual Acuity Outcomes: Although there was a transient dip in best-corrected visual acuity (BCVA) involving a brief reduction of 7.4 letters post-implantation, the overall stability or slight improvement in BCVA in the treatment group is notable. In contrast, the control group experienced a decline, underscoring the potential benefits of newer treatment modalities.
- Safety Profile: The safety analysis identified a few ocular adverse events, such as cataract and vitreous hemorrhage, which occurred in roughly 16.2% of the treatment group. While these numbers are relatively low, clinicians and patients alike must carefully consider all small distinctions when weighing the benefits against the risks.
The trial’s results provide strong footing for considering continuous drug delivery not only as an effective treatment but also as a patient-friendly alternative to standard anti-VEGF injections.
Addressing the Tricky Parts: Safety, Efficacy, and Patient Considerations
Every new treatment comes with its own set of twisted issues and tangled considerations. While the clinical outcomes of Susvimo are promising, healthcare professionals must take a closer look at the broader picture—focusing on both the fine points of its efficacy and the subtle details of its safety profile.
Balancing Efficacy and Safety
From the data provided by the Phase III Pavilion trial, it is abundantly clear that Susvimo delivers significant improvements on the DRSS. Nevertheless, the intricate parts of treatment efficacy also include monitoring for any adverse effects that might emerge long-term. The slight unpredictable dip in visual acuity observed shortly after implantation is something that requires further attention. However, it is encouraging that these changes resolved within eight weeks.
It is essential to recognize that every novel therapy comes with a period of adjustment as both clinicians and patients figure a path through the new treatment landscape. Here is a brief overview of the pros and cons:
-
Pros:
- Extended treatment intervals mean fewer procedures and less disruption to daily life.
- Sustained drug delivery may lead to a more consistent therapeutic effect.
- Reduces the likelihood of missing appointments, a common issue in the management of chronic conditions.
-
Cons:
- The implantation procedure and potential for early transient visual changes need careful monitoring.
- Some ocular adverse events, although statistically low, remain serious and need to be openly discussed with patients.
- The long-term durability beyond the one-year trial period is yet to be fully understood.
These bullet points help to crystallize the small distinctions and hidden complexities involved in switching from a conventional treatment strategy to a continuous drug delivery system.
Understanding Patient Perspectives and Quality of Life Improvements
Patients living with diabetic retinopathy often face an overwhelming treatment journey. Beyond the clinical metrics, there is the human experience tied to repeated visits, invasive procedures, and the constant anxiety about potential vision loss. The shift to a therapy that requires just one refill every nine months can reduce these nerve-racking visits and make managing daily life less off-putting.
For many, the constant barrage of monthly injections leads to both physical discomfort and emotional strain. In contrast, a continuous delivery system simplifies the treatment process, allowing patients to focus on maintaining their quality of life. When patients do not have to work around a rigorous injection schedule, they are more likely to adhere to the treatment plan, ultimately leading to better long-term outcomes.
Weighing the Benefits Over Conventional Anti-VEGF Treatments
One of the most notable shifts in diabetic retinopathy management is the contrast in benefits provided by continuous therapy versus traditional anti-VEGF treatments. Whereas former methods require regular, sometimes monthly, injections, newer approaches offer the convenience of a longer treatment cycle which is both key and super important.
Comparative Analysis of Treatment Regimens
When we compare the standard anti-VEGF injections with a continuous delivery system like Susvimo, several beneficial factors emerge:
- Reduced Frequency: Traditional treatments are characterized by frequent visits to the eye clinic, which can be both overwhelming and intimidating for patients. In contrast, a nine-month interval between refills simplifies the medical regimen considerably.
- Stable Drug Levels: Continuous release leads to more stable intraocular drug concentrations, which can potentially offer better control over disease progression. This steady exposure may help address the subtle issues that arise from fluctuating drug levels in conventional therapy.
- Patient Adherence: Extended treatment intervals naturally reduce the likelihood of missed treatments—a problem that can have complicated pieces, including deteriorating vision or delayed intervention during off cycles.
- Potential Long-Term Gains: Although longer-term studies are needed, early indications from the Phase III Pavilion trial suggest that the use of sustained-release implants may contribute to better overall visual outcomes and fewer complications over time.
In many ways, Susvimo may be seen as a paradigm shift in treatment delivery. By offering a less disruptive approach to managing diabetic retinopathy, the therapy opens up possibilities for enhanced patient satisfaction and potentially improved adherence to treatment plans.
How Extended Interval Treatments Support Clinical Efficacy
It is important to recognize that the success of any treatment not only depends on its immediate effects but also on how well it integrates into a patient’s lifestyle. Extended interval treatments like Susvimo address many of the confusing bits associated with more frequent injections. Patients become less burdened by the rigors of continuous medical visits, and clinicians have more time to focus on those with the most pressing needs.
The clinical efficiency of a continuous delivery system also allows for smoother clinical workflows. In practices where appointment scheduling can be a problematic tangle of issues, having fewer scheduled visits benefits both practitioners and patients. The overall shift in patient management could lead to improved outcomes, creating a win-win scenario that was once only dreamed about in the realm of diabetic retinopathy management.
Future Perspectives on Continuous Delivery Therapies in Diabetic Eye Care
As we look ahead, it becomes clear that continuous drug delivery systems represent a significant stride forward in modern ophthalmology. There remains an exciting field of research aimed at enhancing treatment regimens and exploring further applications of sustained-release technology. For instance, newer platforms and implants might not only improve current delivery methods but also open the door to treating other retinal conditions with similar approaches.
The frontier of diabetic retinopathy treatment is ripe for innovation. Research is ongoing to better understand the long-term outcomes associated with continuous delivery, as well as to potentially combine such therapies with emerging approaches from alternative medicine, nutrition, and advanced pharmacotherapy. Each advancement offers the promise of mitigating the twists and turns inherent in managing a chronic disease.
Emerging Trends and Research Areas
Several emerging trends are worth mentioning as we anticipate the future landscape of diabetic retinopathy treatment:
- Next-Generation Implants: As medical technology continues to evolve, we are likely to see even more refined drug-delivery systems that leverage nanotechnology or biodegradable materials to further minimize the need for invasive procedures.
- Personalized Medicine Approaches: Future treatment regimens may incorporate genetic markers and personalized diagnostics to tailor continuous therapy to an individual’s unique disease progression and overall health profile.
- Integration with Telemedicine: The surge in telemedicine offers a unique opportunity for remote monitoring of patients, ensuring that any subtle parts or small distinctions in patient response can be quickly identified and addressed.
- Combination Therapies: There is potential to combine continuous drug delivery with other treatment modalities, such as dietary modifications, lifestyle interventions, and complementary alternative therapies, enhancing overall therapeutic benefits.
These evolving strategies underpin the importance of a holistic view in the future of diabetic retinopathy management. Through close collaboration between clinical researchers, practitioners, and technology developers, there is a bright future ahead where the hurdles of current treatments can be overcome, making the management of diabetic retinopathy a less complicated piece for everyone involved.
Implementing New Continuous Therapies in Clinical Practice
While the promise of a sustained anti-VEGF implant is exciting, actual implementation in clinical practice involves its own set of tricky parts. For instance, physicians must get into the details of patient eligibility and thoroughly explain the benefits and potential complications associated with new treatment technologies.
Clinical adoption of new therapies like Susvimo is not without its challenges. Several factors play into whether a new treatment will be embraced widely:
- Training and Familiarization: Ophthalmologists and retinal specialists require proper training to master the implantation technique. Getting around these learning curves involves managing your way through hands-on workshops, comprehensive training sessions, and continued medical education.
- Cost and Reimbursement Issues: New medical technologies often come with higher initial costs. Over time, however, if the therapy proves to be more efficient and reduces the need for frequent follow-ups, those costs may be offset by better long-term patient outcomes.
- Patient Education: Patients need to understand why a continuous delivery system may be superior to traditional injections in terms of reduced treatment frequency and better quality of life. Clear, accessible communication that outlines the benefits and addresses potential fears is essential.
- Monitoring and Follow-Up: Although extended treatment intervals are beneficial, they also require a robust system for monitoring the patient’s overall ocular health. Digital health platforms and remote monitoring systems can play a key role in ensuring any subtle changes in the patient’s condition are caught early.
By embracing these practical steps, clinics can make your way through the layers of adopting continuous therapies, ensuring that both patients and healthcare providers benefit from this promising advancement.
Best Practices for Transitioning to Continuous Drug Delivery
Here are a few best practices that clinicians might consider when integrating continuous drug delivery into their treatment protocols:
- Rigorous Pre-Procedure Assessments: Evaluate patient history and prior responses to conventional anti-VEGF injections. Thorough patient screening is essential to ensure that the continuous delivery system is the right fit.
- Comprehensive Patient Counseling: Help patients understand the benefits, including the fewer injections and more stable treatment outcomes, all of which contribute to a better quality of life.
- Regular Post-Implantation Monitoring: Even though the extended refill cycle is beneficial, it remains crucial to conduct regular follow-ups. Use both in-person assessments and telemedicine check-ups as complementary strategies.
- Collaborative Decision-Making: Foster a collaborative environment where patient feedback informs ongoing treatment adjustments. This helps in addressing any hidden complexities or small distinctions that might arise during treatment.
Transitioning to continuous drug delivery systems necessitates not only clinical readiness but also patient confidence. When patients feel supported throughout the process, the likelihood of a successful treatment outcome significantly improves, creating a more favorable atmosphere for everyone involved.
The Ripple Effects on Public Health and Community Impact
Beyond individual patient benefits, new therapies such as Susvimo have broader implications on public health. With diabetic retinopathy affecting millions of people—many of whom are already dealing with multiple health challenges—the availability of less disruptive, more efficient treatments could reduce the overall burden on healthcare systems.
When fewer clinic visits are required, available healthcare resources may be reallocated to address other pressing needs. This improved efficiency is especially important in communities where access to specialized eye care is limited. Ultimately, extended interval treatments can lead to a more balanced and manageable healthcare scenario, where both patients and practitioners have more room to find their path through various treatment challenges.
Community and Societal Benefits
The benefits of continuous drug delivery systems extend well beyond the individual level. For society, the shift toward more streamlined, patient-friendly treatments offers several key advantages:
- Improved Adherence to Treatment: With fewer appointments and less frequent treatments, patients are more likely to stick with their prescribed therapy, leading to better long-term outcomes and reduced overall healthcare costs.
- Reduced Healthcare Burden: A decrease in the number of monthly interventions translates to less stress on healthcare facilities, allowing these institutions to reassign resources where they are most needed.
- Economic Benefits: Fewer doctor visits can result in lower cumulative costs for both patients and the healthcare system, paving the way for more sustainable patient care.
- Enhanced Patient Satisfaction: Continuous drug delivery systems create a more positive patient experience, which can lead to higher satisfaction rates and better overall community health outcomes.
These ripple effects emphasize that innovations in treatment do not exist in a vacuum—they have the power to shape public health strategies and improve quality of life on a broader scale.
Final Thoughts on the Future of Diabetic Retinopathy Management
As we stand on the brink of a new era in diabetic retinopathy treatment, it is clear that continuous delivery systems such as Roche’s Susvimo mark a turning point in modern ophthalmology. This new therapy, with its promise of extended treatment intervals and improved patient outcomes, highlights the importance of embracing advanced technologies that put patients first.
While there are still tangled issues to sort out from a clinical perspective—such as early transient visual changes and the need for ongoing monitoring—the overall benefits of fewer clinic visits and sustained drug efficacy present a compelling case for broader adoption. The emerging trend is one that seeks to simplify complicated pieces of contemporary treatment regimens, ultimately offering more predictable and manageable solutions for diabetic retinopathy.
In the coming years, continued research and real-world data will further illuminate the role of continuous delivery systems in managing complex retinal conditions. It is both exciting and reassuring to witness the efforts of researchers, clinicians, and medical innovators as they take on the challenge of transforming patient care. As we figure a path through these advancements, one thing remains certain: the pursuit of therapies that combine clinical efficiency with enhanced quality of life is a journey well worth taking.
Looking Ahead: A New Dawn for Ophthalmic Innovation
The introduction of continuous drug delivery options has opened up a promising chapter in the management of diabetic retinopathy. As healthcare providers get into the details of each patient’s unique needs, they can now consider an array of treatment options that reduce the stressful frequency of injections and offer more stable drug delivery mechanisms.
By aligning clinical practice with patient-centric innovations, we move closer to an era where the management of diabetic retinopathy is less intimidating and inherently more supportive of the patient’s lifestyle. Future studies will help us drill down into the fine points of long-term safety and efficacy, ensuring that this revolutionary approach continues to evolve in line with both technological advancements and patient expectations.
Embracing Change and Enhancing Patient Outcomes
The journey toward improved treatment outcomes for diabetic retinopathy is filled with both promise and challenging bits. The positive results from the Phase III Pavilion trial provide strong evidence that continuous delivery systems can mitigate many of the nerve-racking aspects of traditional therapies. However, no treatment is entirely without complications. Healthcare professionals must continue to work through the issues that arise along the way, ensuring that every patient receives individualized care that addresses the fine shades of their condition.
As we continue to adopt and refine these innovative therapies, collaboration between research scientists, pharmaceutical companies, and clinical practitioners will be indispensable. By staying flexible, educating patients effectively, and embracing technology, we can ensure that every patient facing diabetic retinopathy is given the best possible chance at preserving their vision and improving their overall quality of life.
Conclusion: The Promise of Continuous Delivery in Diabetic Retinopathy
In conclusion, the approval of Roche’s Susvimo for diabetic retinopathy represents more than just a new treatment option—it signals a broader shift in the way we approach chronic ocular diseases. By reducing treatment frequency, offering sustained benefits, and addressing both the practical and psychological needs of patients, continuous drug delivery therapies are poised to revolutionize diabetic eye care.
Though there are still complicated pieces and fine points to address, the potential for improved patient outcomes and a simplified treatment regimen offers a hopeful glimpse into the future of healthcare. As we dig into the details and work through the small twists and turns of implementation, the overarching goal remains clear: to find effective, patient-friendly treatment options that enhance quality of life and safeguard vision.
With continued innovation, thoughtful integration into clinical practice, and patient-centric care at the forefront, solutions like Susvimo could well become the gold standard in managing diabetic retinopathy. It is up to all stakeholders in healthcare—from clinicians to researchers—to embrace these advancements and work together to make the promise of continuous, sustained therapy a reality for millions of patients worldwide.
This editorial is not just an analysis of a new treatment modality; it is a call to action for the medical community. By recognizing the tangible benefits and carefully addressing the associated challenges, we have the opportunity to reshape the landscape of diabetic eye care for the better. The journey ahead might be full of problems and loaded with issues, but, as history has shown, such challenges often lead to the most groundbreaking innovations in medicine.
Ultimately, as we figure a path through these changes, the impact on both individual patients and the broader healthcare system will be significant. By reducing the need for frequent invasive procedures, enhancing overall treatment adherence, and fostering a more patient-friendly environment, continuous delivery therapies stand to redefine what is possible in the management of diabetic retinopathy.
Let us embrace this evolution with a spirit of optimism and determination, confident that each step forward is a stride toward a future where vision loss from diabetic retinopathy is no longer inevitable but, instead, manageable and even preventable.
Originally Post From http://www.pharmexec.com/view/fda-approves-roche-susvimo-diabetic-retinopathy
Read more about this topic at
Persistence of vision
Regenerating Eye Tissues to Preserve and Restore Vision