Assessing the State of NHS Cancer Diagnosis: An Urgent Look at Patient Outcomes
The latest league tables ranking NHS hospital trusts in England have laid bare a critical challenge in our healthcare system. With almost three-quarters of trusts failing to meet key cancer targets, it is high time that we take a closer look at the implications of these delays for patients battling what is, after all, the UK’s leading cause of death.
In this opinion piece, we will dig into the data, explore the tricky parts of meeting cancer targets, and discuss the broader implications of delays in diagnosis and treatment. We will also take a closer look at how these delays are affecting patient outcomes, the pressures placed on NHS trusts, and the urgent need for government action to provide faster, more efficient care.
Understanding the Tricky Parts of NHS Cancer Targets
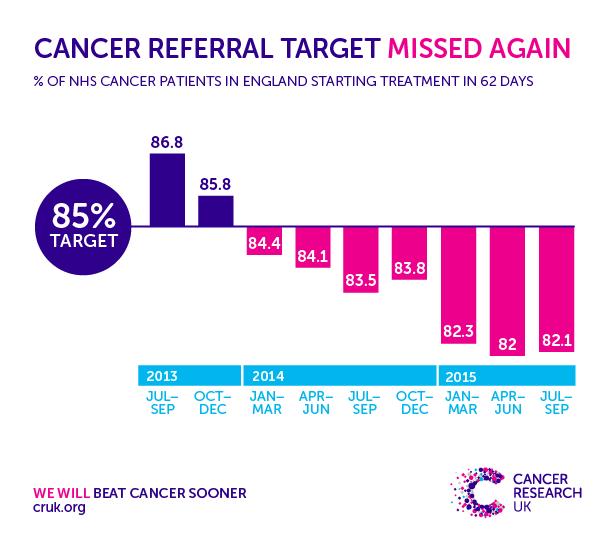
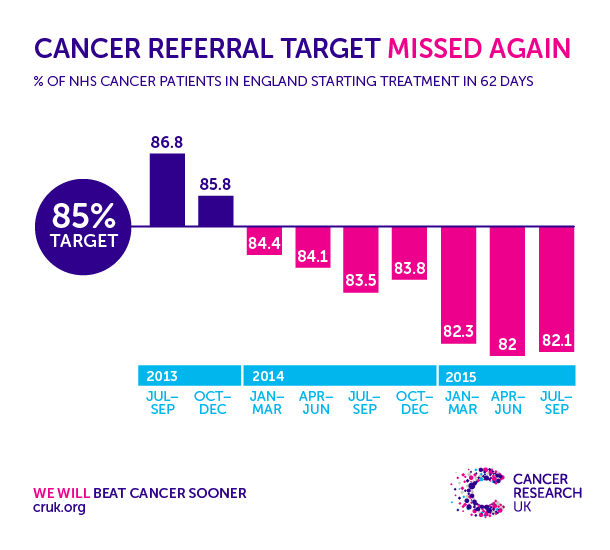
The fresh analysis indicates that roughly 76% of NHS trusts are missing the target of ruling cancer in or out within 28 days for at least 80% of urgent referrals. Likewise, around 73% of trusts do not begin treatment within the required 62-day period for 75% of patients. These statistics, pulled directly from the recently released league tables, reveal more than just numbers—they highlight real-world implications for patients and families waiting for critical diagnoses and treatment interventions.
There are several tangled issues involved when we talk about cancer targets:
- Diagnostic Delays: Prompt diagnosis is paramount. A delay of even a few days can turn what might seem like a narrow timeframe into a nerve-racking ordeal for patients and their loved ones.
- Treatment Initiation: Waiting for treatment not only exacerbates patient anxiety but also, in many cases, reduces the window of opportunity for effective intervention.
- Resource Allocation: Limited resources, staffing shortages, and infrastructural constraints contribute to these delays, making it difficult for the system to consistently hit all the right marks.
The metrics being used—28 days for diagnosis and 62 days for treatment—are not just bureaucratic benchmarks. They serve as essential indicators of how well NHS trusts are performing in bringing down waiting times and ensuring patients receive timely care. When these targets are missed, it is a clear sign that the system’s mechanisms for rapid response are falling short.
Delving Into the Data: A Closer Look at Diagnosis and Treatment Delays
When examining the data, we find that the usual suspects behind delays are not always operating in isolation. Rather, they are part of a system-wide issue that limits how effectively hospitals can manage their patient loads. Consider the following table summarizing the performance of certain trusts:
| Trust Name | Diagnosis within 28 Days (%) | Treatment within 62 Days (%) |
|---|---|---|
| Mid and South Essex NHS Foundation Trust | 59.2% | 42.2% |
| Hull University Teaching Hospitals NHS Trust | 57.5% | 49.3% |
| Calderdale and Huddersfield NHS Foundation Trust | — | 87.3% |
| Bolton NHS Foundation Trust | 88.6% | — |
This table highlights generally how some trusts struggle with rapid diagnosis and treatment start times. On one end, we have trusts that are managing to meet or come close to meeting the targets, while others lag behind significantly.
What does this mean for patients? For many, one of the hidden complexities of cancer care is the wait—waiting for a diagnosis, waiting to find out whether a lump is benign or malignant, and waiting for the start of treatment. These waiting periods, filled with uncertain moments and nerve-racking delays, can have profound impacts on both the physical and emotional well-being of patients.
How Delays in Cancer Diagnosis Impact Patient Outcomes
The issue of delayed diagnosis and treatment is more than just a matter of statistics; it is a matter of life and death. When the system fails to live up to its own targets, the following implications emerge:
- Reduced Treatment Options: The longer cancer remains undiagnosed or untreated, the narrower the range of therapeutic interventions becomes. This often translates to a lower chance of successful treatment.
- Worsened Prognosis: Early intervention is a critical factor in enhancing survival rates. With delays, patients can sometimes face a situation where the disease has advanced to a more severe and less manageable stage.
- Psychological Burden: The period of uncertainty has its own challenges. The waiting game keeps patients and their families in a state of anxiety, stress, and fear—sentiments that are difficult to quantify but all too real.
Experts in the field are clear: delays in both diagnosis and treatment can lead to fewer viable treatment options and, ultimately, a higher likelihood of premature death. The targets set for 28 days (to diagnose) and 62 days (to begin treatment) are not arbitrary—they are super important milestones meant to ensure that patients receive the rapid care needed for a better chance at recovery.
Exploring the Government’s Role in Enhancing Diagnostic Speed
Given the current statistics, concerns have been raised about how the government and NHS administrators are addressing the issue. The health secretary has suggested that these league tables serve as a mirror, reflecting the areas that require urgent support. Despite these assertions, there is considerable debate about whether the current measures are sufficient to meet the needs of an ever-growing patient base.
Critics argue that while the league tables shine a light on deficiencies, more must be done to sort out the following challenges:
- Funding Shortfalls: Without increased financial input, it is difficult to expand diagnostic services, hire more staff, or upgrade essential equipment.
- Infrastructure Improvements: Many NHS trusts operate within facilities that are not optimally designed to handle the current patient overwhelms. Expanding and modernizing these facilities is critical.
- Staffing and Training: There has been consistent concern about the shortage of trained healthcare professionals, particularly those who specialize in oncology. Investing in workforce development could go a long way in reducing waiting times.
Government strategies should focus on these key areas by setting aside dedicated funding, exploring public–private partnerships, and implementing policy changes that empower hospital trusts to make rapid improvements in service delivery.
Reducing Treatment Delays: The Importance of Effective Resource Management
Improving cancer care outcomes depends largely on how well NHS trusts manage their resources. Currently, many healthcare facilities find themselves tangled in issues like high patient volumes, technological limitations, and under-resourced diagnostic departments.
Some of the effective measures that can be taken to reduce treatment delays include:
- Enhanced Scheduling Systems: By upgrading digital scheduling and referral systems, trusts can figure a path to more efficient patient processing, ensuring that no one waits unnecessarily long for evaluation.
- Streamlined Diagnostic Procedures: Integrating and standardizing diagnostic protocols can help reduce variability in care and ensure that every patient is processed quickly and accurately.
- Investing in Diagnostic Technology: Modern diagnostic equipment not only speeds up tests but can also improve accuracy, minimizing the need for repeat tests that contribute to delays.
These interventions, while seemingly simple, represent a complex set of challenges in practice. It is critical to understand that improvements in resource management go hand in hand with changes in policy and funding approaches. The government must work closely with NHS hospital trusts to address these issues on a system-wide level.
Enhancing Cancer Patient Safety in a Changing Healthcare Landscape
Cancer care is not only about diagnosis and treatment—patient safety is an essential part of the conversation. When dealing with something as delicate as cancer treatment, protecting patients from potential hazards that arise from delays or mismanagement can be quite intimidating.
Ensuring high standards of patient safety should involve:
- Regular Performance Monitoring: Routine audits and performance reviews of hospital trusts can help identify problematic areas early on. Transparency in these metrics is key.
- Patient Feedback Mechanisms: Collecting and acting on patient feedback can shine a light on areas that require improvement, ensuring that patient voices are heard in the decision-making process.
- Training Programs: Continuous professional development for healthcare workers helps them stay abreast of the latest protocols and technological advancements, which in turn improves patient safety.
When hospital trusts actively work to uphold patient safety, it not only builds trust between providers and patients but also improves overall outcomes. Creating an environment loaded with issues only serves to exacerbate existing delays and, worse still, may compromise the quality of care patients receive.
Improving Communication and Transparency Within the NHS
One of the most important, yet often overlooked, aspects of timely cancer care is communication. For patients navigating the maze of cancer care, staying informed can make the twists and turns of the process a little less daunting.
There is a growing call for better communication strategies within the NHS. This could include:
- Clear Reporting Standards: More consistent reporting on performance measures can help patients know what to expect when they seek care.
- Direct Channels for Patient Queries: Establishing robust helplines or digital platforms where patients can get real-time updates on their status could dramatically reduce uncertainty and stress.
- Timely Updates on Changes in Protocol: Whether it is due to a shift in staffing or changes in clinic hours, ensuring that patients stay informed about any disruptions in service is crucial.
By finding your way through these communication challenges and ensuring transparency at every level, the NHS can improve trust and empower patients to take a more active role in their care. Clear information, even if it highlights areas that need improvement, works as a foundation for change.
Case Studies: Reflecting on Trust Performances in Cancer Care
Individual trusts have shown varying degrees of success in meeting cancer targets. For instance, while some trusts like Bolton NHS Foundation Trust have excelled in the 28-day diagnostic target, others like Hull University Teaching Hospitals NHS Trust have significantly lagged in both diagnostic and treatment targets. These disparities raise a crucial question: what distinguishes better-performing trusts from those struggling to meet the targets?
In reviewing these case studies, several common themes emerge:
- Efficient Use of Technology: Trusts that have invested in updated technological solutions for scheduling and diagnostics tend to perform better. Their digital systems are designed to take a closer look at the fine points of patient flow and optimize the process accordingly.
- Proactive Staffing Solutions: In facilities where ongoing professional training and adequate staffing levels are prioritized, the system is better equipped to manage high patient volumes without compromising on the speed of diagnosis and treatment.
- Integrated Communication Protocols: Successful trusts have implemented dedicated channels to ensure that all stakeholders—from clinical staff to administrative personnel—are on the same page regarding patient care, leading to fewer missteps and delays.
These case studies demonstrate that improvements are possible. They show that by working through the tangled issues of resource constraints and communication breakdowns, it is feasible to hit ambitious diagnostic and treatment targets consistently.
Government Strategies for Bolstering Cancer Patient Safety
The role of government in this matter cannot be understated. The health secretary has indicated that the league tables are a step toward identifying where local services are not meeting the necessary benchmarks. However, these figures also paint a picture of a system that is, in many respects, full of problems and obviously in need of urgent reform.
Policy-makers can consider several strategies to move forward:
- Targeted Funding Initiatives: Allocating funds specifically for upgrading diagnostic and treatment equipment can accelerate progress. This targeted approach would help trusts that are currently struggling to upgrade their facilities.
- Performance Incentives: Instituting performance-based incentives can motivate hospital trusts to strive for excellence in patient care. This offers the dual benefit of public accountability and direct rewards for improvement.
- Cross-Trust Collaboration: Encouraging trusts that are performing well to share best practices and training protocols could help elevate the overall standard of care across the board.
These measures require a thoughtful approach from both the government and NHS administration, balancing short-term needs with long-term planning. By fostering an environment where improvement is constantly encouraged, the system can begin to address the current shortcomings in patient care.
Patient Perspectives: Life in the Waiting Room and Beyond
Behind every missed target statistic is an individual patient and often an entire family grappling with uncertainty. The human cost of these delays is substantial and cannot be brushed aside as mere numbers in a report. For patients, the waiting room is not just a physical space—it is a reminder of how critical time is when facing a life-threatening illness.
Patients have voiced their concerns in various ways, ranging from personal testimonials to organized campaigns demanding faster service. Their experiences offer several insights into the gravity of the situation:
- Emotional Stress: The prolonged waiting periods lead to significant anxiety and stress, as patients and their families face the challenging twists and turns of what might seem like endless delays.
- Trust in the System: Every delay chips away at the confidence that patients have in the NHS. Restoring this trust is key to ensuring that individuals continue to seek care without unwarranted hesitation.
- Impact on Daily Life: The ripple effects of waiting—missed work, disrupted family life, and intensified emotional strain—are factors that further complicate an already nerve-racking ordeal.
Understanding these patient perspectives is essential for any meaningful discussion about healthcare reform. Efforts to overhaul the system must keep the patient experience at the core, ensuring that every policy change or funding boost translates into tangible benefits for those in need.
Looking Forward: Setting the Course for a More Responsive NHS
The coming years are critical for transforming how cancer care is delivered in England. It is not enough to merely highlight shortcomings through league tables and reports. We must work together—clinicians, administrators, patients, and government—to figure a path that alleviates the current delays and fosters a system where prompt diagnosis and treatment are the norms rather than the exceptions.
Key steps in this journey include:
- Investing in Infrastructure: An overhaul of hospital facilities, including expanded diagnostic centers and upgraded technology, could help shorten diagnosis and treatment times dramatically.
- Emphasizing Preventive Measures: In addition to reactive care, a more robust focus on preventive screening and early detection initiatives should help reduce the number of cases that reach advanced stages.
- Encouraging Multi-Disciplinary Collaboration: Breaking down the silos that often exist in healthcare can ensure that every facet of care—from primary referral to specialist treatment—is integrated seamlessly.
- Maintaining Accountability and Transparency: Continued publication of performance data, combined with open communication channels, will be critical in ensuring that improvement is sustained over time.
Efforts in these areas will require persistence and dedicated leadership at every level of the healthcare system. They must be underpinned by a strong commitment to patient care that goes beyond meeting bureaucratic benchmarks.
Conclusion: The Time for Action Is Now
The challenges we face with respect to cancer diagnosis and treatment in our NHS are complicated pieces of a larger puzzle. With almost three-quarters of trusts missing their targets, the time has come for decisive and coordinated action. Every persistent delay, every overlooked opportunity, has a direct impact on lives—lives that could be saved through early and effective intervention.
While there are certainly bright spots within the system, as evidenced by trusts that perform well on diagnosis and treatment speed, these examples underscore that improvement is possible. The government, healthcare administrators, and the NHS community must work together to sort out the twists and turns that currently impede fast, effective care.
This is not an issue that can be set aside as just another statistic or a temporary setback. It is a call to action—a reminder that when cancer is involved, every day, every hour, and every minute count. Ensuring that the system is responsive, transparent, and properly resourced is super important, not only to meet targets but to truly safeguard the lives of those in need.
Now is the time for the NHS and policymakers to take decisive steps that will, over time, reduce the waiting periods for diagnosis and treatment, enhance patient safety, and restore public trust in our healthcare system. Only then can we create a system that not only meets the benchmarks on paper but, more importantly, delivers the high standard of care that every patient deserves.
Originally Post From https://www.theguardian.com/society/2025/sep/14/hospitals-england-failing-to-hit-cancer-targets-league-tables
Read more about this topic at
Three in four English hospitals failing to hit two cancer …
Cancer patients shun crisis-hit NHS to go private