Innovative Radiomodulation Approaches for Tackling Alcohol Use Disorder
Alcohol use disorder (AUD) remains a tricky public health problem, with many patients facing overwhelming challenges in achieving lasting sobriety. With traditional treatments often showing tangled issues and high relapse rates, there is a growing interest in alternative non-invasive therapies that can steer through these complicated pieces. In this opinion editorial, we examine the evolving role of radiomodulation as a therapeutic option, focusing on its use in targeting the nucleus accumbens (NAc) for alleviating AUD symptoms. We also compare this novel approach with deep brain stimulation (DBS) and other conventional therapies.
Understanding the Nucleus Accumbens and Its Role in Addiction
At the heart of addiction research is the nucleus accumbens, a key component of what many refer to as the brain’s reward system. This small brain structure plays a super important role in reinforcing behaviors that lead to dependency. The NAc is especially known for its involvement in processing high levels of dopamine, which drives cravings and maladaptive reward-seeking behaviors that many patients with AUD experience daily.
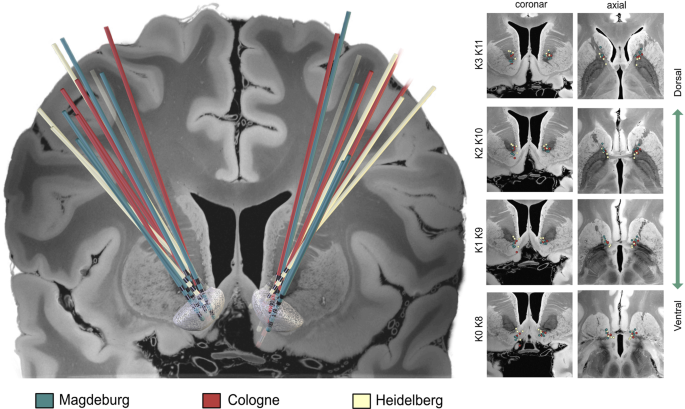
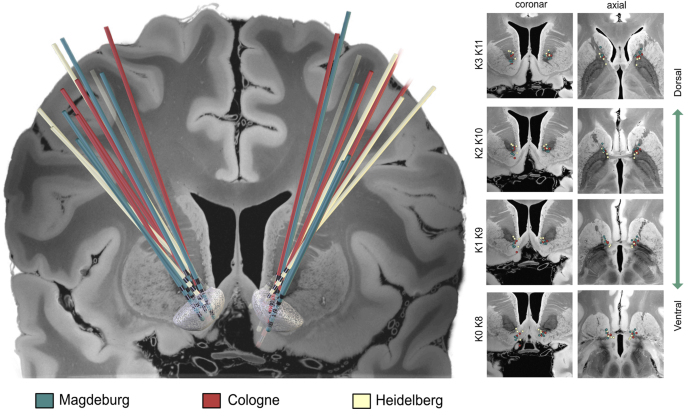
NAc Anatomy: The Core and Shell Dichotomy
The NAc is divided roughly into two parts: the core and the shell. Each of these regions has its own subtle details in terms of cellular composition and connections with other brain areas. The shell, with its extensive dopaminergic connections to the ventral tegmental area (VTA), is deeply involved in the emotional aspects of addiction, while the core is aligned more with motor functions and motivation. Some argue that radiomodulation may yield better results when directed at the NAc shell than at its core, given the shell’s role in managing alcohol-triggered cravings.
Key Challenges in Current AUD Treatments
Even with progress in pharmaceutical and behavioral treatments, many aspects of AUD therapy remain on edge due to the myriad of surgical, technical, and emotional challenges facing patients. Invasive approaches like DBS, for instance, come with their own nerve-racking complications. Surgical complications, device malfunctions, and post-operative infections are among the issues that have left both clinicians and patients searching for alternatives that might reduce these risks.
Invasive vs. Non-Invasive Approaches
The major difference between invasive procedures like DBS and emerging non-invasive techniques such as radiomodulation lies in their risk profiles and recovery times:
- DBS involves surgical electrode implantation, which can be intimidating due to its potential for infection, hemorrhage, and hardware issues.
- Radiomodulation, on the other hand, uses sub-ablative doses of ionizing radiation delivered with high precision, avoiding the nerve-racking risks associated with surgery.
- Patients who are not ideal candidates for surgery may benefit significantly from these non-invasive strategies.
Radiomodulation: The Science and Its Potential
Radiomodulation is a relatively new concept that involves the delivery of focused ionizing radiation in a way that modulates neural activity without necessarily causing the cell death associated with traditional ablation techniques. Instead of permanently destroying tissue, radiomodulation aims to tweak the balance of neurotransmission in specific brain circuits, thereby promoting long-term therapeutic changes.
Mechanisms of Radiomodulation in the NAc
When we take a closer look at how radiomodulation might work for AUD, the focus is primarily on the effects of radiation on the delicate neuronal circuits within the NAc—especially within its shell. The therapy’s objective is to restore balance by modulating GABAergic and dopaminergic networks, which are known to become unbalanced with chronic alcohol use.
Here are some key points that illustrate the underlying mechanisms:
- Synaptic Plasticity: Moderate radiation doses (typically below 40 Gy) have been shown to induce plastic changes without causing significant structural damage. This means the radiation may help rewire neural circuits by stabilizing or slightly reducing the overactive firing of neurons.
- GABAergic and Dopaminergic Balance: By modulating the response of inhibitory neurons and downregulating excessive excitatory signaling, radiomodulation might effectively dampen the hyperactivity caused by chronic alcohol exposure. This is especially helpful during withdrawal periods when the brain is reeling from an imbalance.
- Permanent or Long-Lasting Effects: Unlike other non-invasive techniques such as transcranial magnetic stimulation (TMS) or transcranial direct current stimulation (TDCS), radiomodulation carries the potential for durable effects after just a single session.
Preclinical and Clinical Evidence
Early studies in animal models have suggested that radiomodulation can lead to significant changes in neuronal firing rates, with reductions lasting for several months. Experiments in mice and even in pig models have shown that low-dose radiation can alter the mesolimbic pathways that underscore addictive behaviors. These findings serve as a stepping stone for larger clinical trials aimed at evaluating the safety and efficacy of this method for treating AUD.
Clinical Comparisons: DBS Versus Radiomodulation
| Parameter | Deep Brain Stimulation (DBS) | Radiomodulation |
|---|---|---|
| Surgical Risk | High (infection, hemorrhage) | Minimal (non-invasive) |
| Procedure Duration | Multiple surgeries and follow-ups | Single session treatment possibility |
| Impact on Neural Circuitry | Localized modulation, but device-dependent | Potential for circuit-wide modulation with lasting changes |
| Patient Suitability | Limited to those who are surgical candidates | Wider applicability given lower risks |
Benefits of a Non-Invasive Treatment Paradigm
Many patients find the idea of neurosurgery intimidating. The mere thought of undergoing invasive procedures can feel overwhelming and off-putting. Radiomodulation offers a key alternative that avoids these scary aspects, making it an appealing option for patients who have limited surgical options or who prefer to bypass the risks associated with implanted medical devices.
Fewer Surgical Complications
Since radiomodulation does not require opening the skull or implanting hardware, it minimizes many of the complications seen with DBS. The absence of incisions and electrodes reduces the risk of infection and lessens the nerve-racking burden of long-term device maintenance. For patients who have comorbid conditions or are generally at a higher risk when it comes to surgery, this non-invasive approach is a beacon of hope.
Potential for Rapid Recovery
Another advantage of radiomodulation is the possibility of a faster recovery compared to invasive surgeries. Without the need for hospital stays or lengthy recovery periods, patients might be able to get back to their daily lives more quickly. This is particularly important when considering mental health, where prolonged recovery times can add stress and diminish overall quality of life.
Enhanced Accessibility and Cost-Effectiveness
Given the significant costs associated with surgical procedures and the extensive follow-up care required for DBS, radiomodulation may also offer a more accessible and cost-effective solution. Without the requirement for surgical suites, recovery time, or expensive implanted hardware, non-invasive radiomodulation has the potential to reach a broader patient base who might otherwise be left without viable treatment options.
Digging Into Current Research and Future Directions
While there is promising preclinical evidence and some early clinical reports on NAc-DBS pointing to potential benefits for alcohol use disorder, the application of radiomodulation is still an evolving area. Researchers are keen to understand the fine points of how sub-ablative radiation doses interact with the delicate balance of excitatory and inhibitory neurotransmission in the NAc.
Ongoing Research: What We Know So Far
Early experiments suggest that radiomodulation, by using sub-lesional doses of radiation, can gently tune the activity of neurons. Researchers have observed changes in the firing rates of key neuronal populations—findings that hint at a durable rebalancing of neurotransmission and a reduction in the cravings that characterize AUD. Some studies even suggest that the impact of radiomodulation could be sustained for months after a single session.
Key Challenges and Future Research Needs
Despite these encouraging results, there are still several tangled issues that need to be sorted out before radiomodulation can become a mainstream treatment for AUD. Here are some of the main areas where additional investigation is needed:
- Dosing Optimization: One of the trickiest parts is finding the optimal radiation dose that will induce the desired changes in neural circuits without inadvertently causing damage. Researchers need to figure a path through this maze of dose-response relationships.
- Long-Term Safety: While early data indicate minimal adverse effects, longer-term studies are essential to ensure that the treatment does not lead to unplanned synaptic plasticity in neighboring regions or adverse astrocytic alterations over time.
- Patient Variability: As with any treatment, individual differences in brain anatomy and the specific manifestations of AUD will likely play a role in determining the success of the procedure. Tailoring radiomodulation strategies to meet the unique needs of each patient remains a full-of-problems challenge.
- Mechanistic Clarity: Although the broad strokes of the biological effects have been mapped out, the little details regarding which neuronal subtypes and glial responses are most affected require further research.
Future Clinical Trials and Their Design
To fully evaluate the potential of radiomodulation for AUD, future clinical trials should adopt comprehensive designs that compare this method directly with both sham procedures and established therapies like DBS. Key outcome measures might include:
- Reduction in alcohol cravings
- Increase in abstinent days
- Changes in neurochemical markers in the NAc
- Quality-of-life assessments during and post-treatment
Properly structured trials will also help clarify whether the long-lasting effects suggested by preclinical research can be replicated in larger, more diverse patient populations.
Practical Considerations and Patient-Centered Impact
When assessing new therapies, it is super important to consider not only their therapeutic potential but also their impact on patients’ daily lives. Radiomodulation, due to its non-invasive nature, has the promise of reducing the physical and psychological burdens that many patients face when undergoing conventional invasive procedures.
Enhanced Patient Comfort and Reduced Anxiety
For many, the idea of brain surgery is off-putting. Radiomodulation allows patients to avoid the nerve-racking environment of the operating room while still potentially benefiting from targeted neuromodulation. The possibility of receiving treatment as an outpatient with minimal recovery time can significantly reduce anxiety and make the treatment more approachable.
Adapting Treatment to Individual Needs
One of the most promising facets of radiomodulation is its adaptability. Given that the NAc comes in two distinct sub-regions—the shell and the core—it is feasible to customize the radiation dose to target the specific areas most heavily involved in alcohol-triggered dopamine imbalances. This personalized approach could allow clinicians to fine-tune the therapy based on the patient’s unique neuroanatomical and clinical profile.
Cost and Accessibility Benefits
Compared to invasive procedures that require expensive surgical skills and long-term hospital stays, radiomodulation may offer a more cost-effective alternative in the long run. Reduced need for post-operative care and fewer complications can translate to lower overall treatment costs, potentially making advanced neuromodulatory therapies accessible to a wider segment of patients.
Reflecting on the Broader Implications for Modern Addiction Therapy
The exploration of radiomodulation as a treatment strategy for AUD comes at a time when modern medicine is increasingly focused on integrating alternative, patient-friendly approaches into mainstream practice. As we consider the current landscape of addiction therapy, it is clear that non-invasive treatments are becoming more attractive—not only for their clinical efficacy but also for the significantly reduced risk profile they offer.
Comparative Insights: Radiomodulation and Other Non-Invasive Techniques
Although techniques like TMS and TDCS have been around for a while, their capacity to target deep brain structures like the NAc is limited. Radiomodulation steps into this challenge by combining non-invasiveness with the ability to deliver near sub-millimetric accuracy. This precision means that even the subtle parts of deep-seated neural circuits can be modulated without causing widespread changes in adjacent brain tissue.
Impacts on Broader Mental Health Treatment
Beyond its application in AUD, the implications of radiomodulation extend to other addiction-related and mood disorders, such as obsessive-compulsive disorder, depression, and anxiety. The intertwined nature of these conditions means that a single therapeutic approach could potentially provide benefits across a range of issues, making it a key area for future research and development.
Key Takeaways for Clinicians and Researchers
For those working at the front lines of addiction treatment, understanding the potential benefits and challenges of radiomodulation is essential. Here are some bullet points summarizing the major insights:
- Radiomodulation targets the nucleus accumbens with sub-ablative doses of radiation, potentially restoring balance in neurotransmitter systems affected by chronic alcohol use.
- The non-invasive nature of radiomodulation offers significant advantages over traditional invasive procedures, including less risk of infection and a quicker recovery.
- Early preclinical studies show promising results in modulating neuronal firing and reducing behavioral indicators of addiction.
- Future research must address dosing optimization, long-term safety, and individual patient variability to fully establish the clinical utility of this approach.
- Radiomodulation’s potential applications may extend beyond AUD to include other neuropsychiatric conditions, increasing its overall relevance in modern clinical practice.
Challenges and Caveats: Moving Forward with Caution
Even the most promising treatments come with their own set of twisted challenges and puzzling bits that need careful attention. Radiomodulation is no exception. While the early data are encouraging, several off-putting issues must be addressed as researchers and clinicians work together to translate these findings into practice.
Individual Variability and Treatment Customization
One of the confusing bits is the fact that not every patient’s brain biology responds the same way to radiation therapy. The subtle differences in how neurons and glial cells react to ionizing radiation can lead to variability in treatment outcomes. To manage this issue, it is essential that future clinical protocols include rigorous screening, personalized dosimetry, and ongoing monitoring.
Potential Unintended Effects
Another tense area revolves around the possibility of unintended synaptic plasticity in regions adjacent to the targeted NAc shell. While sub-ablative doses are designed to avoid cell death, the long-term effects on surrounding tissues, especially glial cells, remain somewhat on edge. Longitudinal studies and careful post-treatment evaluations are critical to ensure that the fine balance of brain chemistry is maintained.
Regulatory and Ethical Considerations
As with any emerging technology, radiomodulation will need to clear regulatory hurdles and address ethical questions. Regulatory bodies will be keen to examine the long-term data to ensure that this promising therapy does not come with hidden, long-term risks. Meanwhile, patient consent processes must thoroughly outline the known benefits and uncertainties, ensuring that individuals fully understand the nerve-racking aspects that might be involved.
Conclusion: A New Frontier in AUD Management
Radiomodulation represents a paradigm shift in the way we approach the treatment of alcohol use disorder. By harnessing the power of targeted, non-invasive radiation technology, clinicians may soon have an alternative tool for resetting the delicate balance within brain circuits that underlie addiction. This approach could offer many of the benefits of deep brain stimulation without the intimidating risks associated with surgical intervention.
In our dive into the subject, we have seen that radiomodulation not only has the potential to reduce alcohol cravings and enhance abstinence rates but also offers the promise of durable, long-lasting effects. The approach is especially appealing given its minimal surgical risk, cost-effectiveness, and potential to be tailored to the individual needs of patients.
That said, much remains to be done before radiomodulation can be adopted into routine clinical practice. Critical challenges such as dosage optimization, ensuring long-term safety, and understanding individual responses need further investigation. As researchers continue to poke around for answers, early data provide a hopeful glimpse into the future of AUD treatment, where non-invasive techniques lead the way in healing and restoring normal neurotransmitter function.
Clinicians, researchers, and policymakers alike must work together to figure a path that balances innovation with caution. Only with careful research and thoughtful implementation will radiomodulation transition from a promising experimental therapy to a super important standard of care for AUD and perhaps other neuropsychiatric disorders.
Final Thoughts
In the face of a condition as persistent and nerve-racking as alcohol use disorder, every new approach that offers hope deserves careful evaluation. Radiomodulation may one day stand as a transformative non-invasive treatment option that helps patients regain control over their lives, overcoming the tangled issues that have long defined addiction. With further research and clinical trials, we hope to see this innovative method provide sustained, meaningful improvements in the quality of life for those affected by AUD.
As we continue to make sense of the fine shades and hidden complexities in the brain’s reward system, radiomodulation inspires optimism that the future of addiction therapy can be both less intimidating and more effective. Now is the time for the medical community to take a closer look, dive in deeper, and ultimately find new ways to bring hope to those who struggle with the heavy burdens of alcohol use disorder.
Originally Post From https://www.cureus.com/articles/368247-nucleus-accumbens-a-therapeutic-target-for-radiomodulation-for-the-treatment-of-alcohol-use-disorder?score_article=true
Read more about this topic at
About Neuromodulation
Neuromodulation: Update on current practice and future …