Digital Transformation in Cancer Care: The Rise of ePROs
Over the past several years, the healthcare industry has witnessed a significant digital transformation, and cancer care is no exception. One development that stands out is the incorporation of electronic patient-reported outcomes (ePROs). This innovative approach is reshaping the way clinicians gather critical information directly from patients about their symptoms and overall well-being. With better communication between patients and healthcare providers, the results have not only led to improved symptom control but have also streamlined the process of adhering to value-based care initiatives.
In recent discussions with leading experts like Dr. Debra Patt from Texas Oncology, we have seen firsthand how the OncoPRO initiative is playing a key role in smoothing the tricky parts of implementing these digital tools. Through collaboration between providers, EHR vendors, and policymakers, ePRO technology is becoming more accessible and user-friendly, even in the face of complicated pieces that previously slowed down its adoption.
This op-ed takes a closer look at the current landscape of ePRO usage in oncology, outlines the obstacles practices face, and examines how dedicated collaborative efforts are creating solutions. We will also explore how these advancements align with critical policy shifts like the CMS Enhancing Oncology Model (EOM) to drive hospital and outpatient facility performance in value-based care.
Overcoming Tricky Parts in ePRO Adoption
Implementing any new digital technology in healthcare often comes with its share of tangled issues and confusing bits. In the realm of ePROs, practices have encountered numerous early challenges that include selecting the right vendor, integrating reporting frequencies, keeping patient participation high, and promptly addressing the feedback received from these reporting tools.
Many clinicians describe the process as nerve-racking initially. The notion of incorporating additional digital tools into their already hectic workflow can feel overwhelming. However, initiatives like OncoPRO are designed to light the way by providing a collaborative hub where these tricky parts can be openly discussed, dissected, and ultimately managed more effectively.
Detailed Breakdown of Challenges
Some of the most common challenges that healthcare professionals face include:
- Vendor Selection: Choosing an ePRO system that integrates seamlessly with existing Electronic Health Record (EHR) systems can be confusing due to the myriad of options available.
- Reporting Frequency: Determining the optimal balance between too frequent and too slack reporting to ensure accuracy without overwhelming patients.
- Patient Engagement: Encouraging consistent and timely reporting by patients, which relies heavily on reminder systems and user-friendly design.
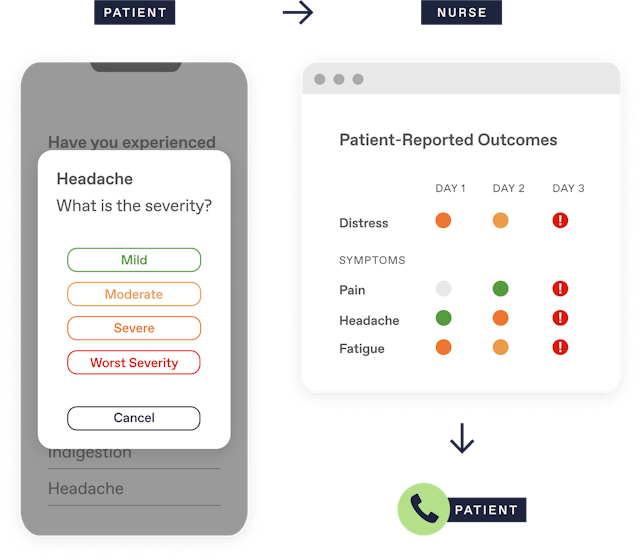
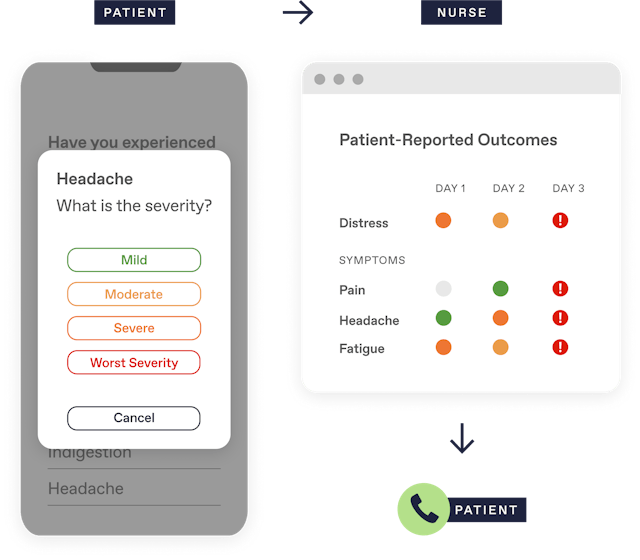
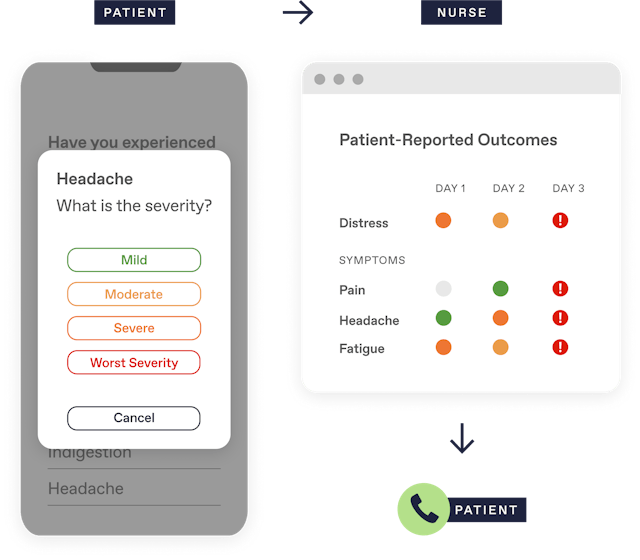
- Response Infrastructure: Establishing a clear and responsive protocol for acting on patient-reported data to prevent escalation of symptoms or complications.
Addressing these issues requires a concerted effort to identify the fine details that make a difference in patient care. When providers, technology vendors, and policymakers come together, they can pool their expertise and resources, making the integration of these systems less taxing and more productive.
Collaboration: The Secret Ingredient to Tackling Complicated Pieces
The OncoPRO initiative is a prime example of how collaboration can help practitioners work through the twists and turns of ePRO implementation. By creating a dynamic community that includes healthcare providers, software developers, and policy experts, this initiative has facilitated an environment where shared experiences are used to fine-tune the process.
During in-depth discussions, experts like Dr. Patt have highlighted several benefits that come from collaborating in this manner:
- Shared Learning: Groups can compare what is working and what isn’t, allowing them to adapt proven strategies quickly.
- Resource Optimization: Instead of each practice starting from scratch, they can leverage collective expertise to make smarter decisions faster.
- Enhanced Systems Integration: Working hand-in-hand with EHR vendors ensures that ePROs are built into the existing systems rather than being an added burden.
- Improved Workflow Design: Collaborative feedback loops help refine the workflow for monitoring symptoms, ensuring that it is both efficient and effective.
This shared approach not only helps tackle the intimidating parts of ePRO implementation but also builds a framework for the long-term sustainability of digital patient care. By fostering teamwork, healthcare organizations can better align with modern value-based care models, sharing the responsibility for patient outcomes while minimizing the impacts of awkward system transitions.
Integrating ePROs into Existing Healthcare Workflows
One of the major hurdles in utilizing patient-reported outcomes effectively is integrating them into current clinical workflows. The separate nature of many ePRO systems means that data can sometimes end up feeling disconnected from the larger health record. This situation creates additional confusing bits for busy clinicians who need immediate access to actionable information.
To address this, practices are putting a significant emphasis on ensuring that ePRO tools are optimized for integration:
- System Compatibility: Ensuring that the ePRO tools work in tandem with pre-existing EHRs to reduce data silos.
- Simplified User Interface: Simplifying the design of the reporting tool, so it remains intuitive enough for both patients and staff to manage without adding extra layers of complication.
- Timely Data Presentation: Making sure that the reported data appears at the clinician’s fingertips immediately, which is key in times when quick decision-making is essential.
Embedding these systems within the existing digital infrastructure not only boosts efficiency but also enhances the overall quality of patient care. When clinicians can easily access patient reports, they can make better-informed decisions, leading to improvements in overall symptom management and patient satisfaction.
Enhancing Patient Engagement to Improve Outcomes
One of the most significant challenges in adopting ePRO systems is ensuring consistent patient participation. Without proper engagement, the quality of the data gathered may suffer, leading to missed opportunities for intervention. Headache-inducing issues such as missed reports, reduced adherence, and ineffective reminder protocols have been well-documented within numerous practices.
Experts like Dr. Patt stress the need for a patient-centric approach when designing and implementing these digital tools. Some strategies that have proven effective in maximizing patient commitment include:
- Automated Reminders: Setting up regular notifications for patients, encouraging them to report how they feel. This approach is particularly useful when combined with user-friendly digital interfaces that minimize the steps needed to submit information.
- Tailored Reporting Schedules: Allowing patients to report both at regular intervals and on-demand ensures they can share critical moments when their symptoms might be escalating.
- User Education: Explaining the benefits and practicalities of ePROs in a clear and accessible manner helps demystify the process and makes the tool less overwhelming.
By taking these steps, practices have seen a remarkable uptick in patient adherence. Not only does this lead to better symptom control, but it also helps reduce the frequency of emergency room visits and hospital admissions, ultimately resulting in a smoother care experience for patients with advanced cancer.
Aligning with Value-Based Care: The Role of ePROs in the EOM Framework
In recent years, federal initiatives like the CMS Enhancing Oncology Model (EOM) have been a major driver behind the shift towards value-based care in oncology. This model emphasizes the importance of outcomes and cost-effectiveness, creating pressure for practices to quickly adopt systems like ePROs. For many institutions, this shift can feel both overwhelming and intimidating.
However, the OncoPRO initiative has provided a roadmap by demonstrating that the added time and effort required for ePRO installation pay dividends in both patient outcomes and operational efficiency. For example, practices see tangible benefits such as improved symptom threshold management, which in turn contribute to reduced hospital stay durations and lower overall treatment costs.
The integration of ePROs with value-based care models has also initiated discussions around reimbursement, especially regarding remote therapy monitoring. As practices delve into the practicalities of charging for these services, many are now exploring remote monitoring codes that align with the work carried out during symptom management.
Table: Benefits of ePROs Aligned with Value-Based Care
| Aspect | Benefit |
|---|---|
| Symptom Management | Enhanced patient monitoring leading to early intervention |
| Operational Efficiency | Streamlined workflows and reduced emergency visits |
| Cost-Effectiveness | Lower overall treatment costs through proactive care |
| Reimbursement Opportunities | Utilization of remote therapy monitoring codes to secure funding |
This table clearly illustrates the multiple benefits that come from the thoughtful integration of ePROs within a value-based care model. The key takeaway for many is that by engaging in collaborative efforts like OncoPRO, practices are making strides towards a more sustainable, quality-focused approach to cancer care.
Strategies to Simplify the Twists and Turns of Workflow Integration
The practical side of integrating ePROs into day-to-day clinical practice cannot be underestimated. Many providers express concerns about how to efficiently figure a path through the challenging steps of implementing a new system while keeping patient care at the forefront.
To address these confusing bits, several actionable strategies have been highlighted by experts who are part of the OncoPRO initiative. Some of these strategies include:
- Mapping the Patient Journey: Developing a standard process workflow that outlines when and how patients are onboarded onto the ePRO platform.
- Embedding Reminders: Utilizing automated reminder systems to prompt patients to report their symptoms at predetermined intervals.
- Adjusting Reporting Frequencies: Experimenting with the timing of reports to find a balance that does not overload patients while still capturing critical data.
- Enhancing Response Protocols: Establishing quick response pathways for patients who report concerning symptoms, ensuring that the right intervention is made in a timely fashion.
By adopting these methods, healthcare practices have been able to smooth out the hidden complexities inherent in integrating new digital tools. The result is a more streamlined workflow, reduced administrative burden, and ultimately, enhanced patient care. The focus remains on making sure that the system is not a barrier but rather a bridge to better health outcomes.
Charting a Path Forward: Lessons from OncoPRO
The experience shared by Dr. Patt underscores the importance of learning and iterating continuously. By gathering real-world insights from a diverse group of practices, OncoPRO has built a repository of best practices that can help others figure a path through similar challenges.
Some of the key lessons include:
- The Importance of Collaboration: Mutual support and shared experiences are essential when confronting the little details that can make or break the success of ePRO integration.
- System Integration Matters: Making sure that the ePRO systems are fully integrated into existing EHRs is super important to avoid redundant work and missed information during patient visits.
- Patient-Centric Design: It is critical to design systems that patients find easy to use, thereby boosting adherence and ensuring accurate, ongoing reporting.
- Continuous Feedback Loops: The willingness to revisit and adjust workflows based on practical experiences can lead to significant improvements in care delivery.
These lessons are not only shaping the current state of oncology care but are also paving the way for future developments. When clinicians, administrators, and technology providers work together, they can tackle nearly every intimidating element that digital health trends throw their way.
Practical Tools and Tips for Digital Symptom Management
As more practices begin to adopt ePRO systems, there is an increased need for practical advice that can assist in day-to-day operations. Clinics have begun incorporating detailed, hands-on strategies to gain traction with the technology. Some tips for practices include:
- Regular Training Sessions: Engage clinicians and support staff in frequent training sessions to get into the nitty-gritty of the system’s functionalities.
- Patient Education Materials: Develop clear and concise guides for patients that explain the process of reporting symptoms and understanding the benefits of ePROs.
- Feedback Channels: Create easy-to-access channels through which both patients and staff can submit feedback on the usability of the platform, helping to identify small distinctions that might impact overall efficiency.
- Monitoring Dashboards: Utilize real-time dashboards to track patient adherence and flag any irregularities in reporting. This proactive measure enables quick intervention when necessary.
Implementing these strategies can feel like steering through a maze at first, but over time, they help establish a robust framework for remote symptom monitoring. The tangible improvements—in everything from reduced ER visits to more strategic patient check-ins—underscore that these efforts are worth the initial challenges.
Global Implications: Shaping the Future of ePRO Implementation
The influence of initiatives like OncoPRO extends well beyond the borders of the United States. Internationally, many healthcare systems are beginning to appreciate the benefits of integrated ePROs. As practices worldwide experiment with digital symptom tracking, the collective experiences reinforce that a patient-centered, collaborative approach is the best way to tackle the twisting turns of any new healthcare technology.
This global perspective is important for several reasons:
- Shared Global Standards: As organizations like ASCO and ESMO develop guidelines for ePRO implementation, an international consensus on best practices is emerging. These guidelines serve as a compass for practices looking to adopt innovative, evidence-based methods in cancer care.
- Cross-border Collaboration: Countries can learn from each other’s successes, especially when it comes to implementing strategies that address tricky parts of patient engagement and integration challenges.
- Economic Efficiency: By standardizing the processes for symptom monitoring and aligning reimbursement codes, healthcare systems can reduce overall costs while improving outcomes.
- Research and Data Sharing: Global collaboration creates an opportunity for large-scale research, providing more robust data on the effectiveness of remote symptom monitoring and patient-reported outcomes.
Ultimately, building an international network of practices dedicated to refining ePROs will generate benefits that echo throughout the global healthcare community, making cancer care more patient-friendly and efficient across diverse health systems.
Steering Through the Future of Cancer Care
As we look ahead, it becomes clear that the integration of ePROs is not just a passing trend but a necessary evolution in cancer care. By working through the complicated pieces of digital health technology, healthcare providers are finding smarter, more efficient ways to take care of patients. The positive outcomes—ranging from reduced hospitalization rates to improved symptom management—demonstrate a concrete return on the effort invested into these systems.
Furthermore, as more practices adopt remote monitoring and enhance their workflows, it is anticipated that reimbursement models will continue to evolve. New remote therapy monitoring codes offer a financial framework that supports these initiatives, reassuring practices that the economic aspects of the transition are being thoughtfully addressed. In this way, the alignment with value-based care initiatives isn’t just beneficial from a clinical standpoint—it also ensures a sustainable financial model going forward.
Real-World Lessons and Emerging Best Practices
The practical insights gathered from OncoPRO illustrate valuable lessons for all stakeholders involved in modern cancer care. Here are some of the real-world best practices emerging from the initiative:
- Dynamic Problem Solving: By regularly exchanging ideas and experiences, practitioners are quickly discovering innovative ways to overcome tangled issues in technology integration.
- User-Friendly Design: Keeping the digital interface simple and intuitive remains a cornerstone of successful ePRO implementation, ensuring that every patient can participate without feeling overwhelmed.
- Timely Interventions: With improved data integration, providers can now find their way to critical information faster, ensuring that interventions are both timely and effective.
- Operational Streamlining: Optimizing the scheduling of symptom reports coupled with automated reminders has succeeded in creating a more efficient and less burdensome workflow for health professionals.
It is clear from these practices that while the adoption of ePROs can initially appear loaded with issues, careful planning and a commitment to collaborative improvement can turn these challenges into opportunities for positive change. Moving forward, organizations will likely refine these strategies further, incorporating continuous feedback to enable even smoother transitions and better outcomes for patients.
Final Thoughts: Embracing Change in Oncology Care
The journey to effectively implementing electronic patient-reported outcomes in cancer care is, without doubt, filled with twists and turns. From selecting the proper vendor to ensuring seamless integration with existing EHR systems, every step of the process requires careful thought and a willingness to adapt. Initiatives like OncoPRO are proving vital by offering a collaborative and supportive network that can help mitigate the intimidating parts of adopting new technologies.
Practices that have embraced these digital tools report significant benefits—not only in clinical outcomes but also in operational efficiency and patient satisfaction. As healthcare providers continue to experiment with and refine these methods, the emerging model of care paints a promising picture of a more integrated, patient-centric approach to managing cancer care in the digital age.
It is imperative for clinicians, administrators, and policy creators to continue working together, pooling their insights to overcome the little details that add up to significant improvements in patient care. As the global healthcare community takes these strides, the future of oncology care looks set to benefit from digital innovation, transforming complex challenges into manageable, systematic procedures that ultimately improve the lives of patients.
Looking Forward: The Ongoing Evolution of ePROs
By fostering an environment that encourages experimentation and collaboration, the journey toward more effective ePRO integration is well underway. As healthcare stakeholders look to the horizon, there is a collective recognition that while the path may be intricate, every advance contributes to a more robust system of care.
Moving forward, we can expect these projects to catalyze significant shifts not just in cancer care but in many areas of healthcare where patient-reported outcomes can make a real difference. Whether it’s through automated reminder systems, user-friendly digital platforms, or streamlined workflows that reduce the busywork associated with traditional reporting, the future is oriented toward making patient care as effective and as compassionate as possible.
For those tasked with managing these transitions, the key lies in embracing change and learning from every experience—both the successes and the setbacks. By continuing to work through the small distinctions that impact daily operations, healthcare professionals can ensure that the adoption of ePROs remains a super important step towards a more integrated, value-driven approach to managing complex diseases like cancer.
Summary: Collaborative Innovation Paving the Way for a Brighter Future
In summary, the digital transformation driven by electronic patient-reported outcomes is fundamentally altering the landscape of cancer care. The practical lessons from the OncoPRO initiative highlight that even the most intimidating aspects of digital integration can be overcome when experts come together to share ideas, strategies, and best practices.
Through dedicated teamwork, continuous learning, and a commitment to easing the tricky parts of technology adoption, clinicians are not only improving symptom management but also paving the way for a more efficient, cost-effective, and patient-centric model of care. As the healthcare community continues to refine these processes and align them with critical value-based care models, the future of oncology—and indeed many other specialties—appears brighter than ever.
Moving forward, it is essential that all stakeholders remain committed to finding actionable solutions for every challenge, no matter how tangled or overwhelming it might seem initially. With persistence, innovation, and collaboration, the next chapter in digital healthcare is one that promises improved outcomes, lowered costs, and a patient experience that truly puts the needs of the individual first.
Concluding Reflections
The field of oncology care is clearly on the cusp of a major shift. With initiatives like OncoPRO leading the way, the integration of ePROs into everyday practice is proving more than just a technical upgrade—it is a transformation that promises to benefit patients, providers, and the entire healthcare system.
By working together to sort out the little details and by embracing the user-friendly aspects of new technology, healthcare providers are turning what was once seen as a nerve-racking challenge into a seamless component of modern care. The use of digital patient-reported outcomes is a testament to the power of collaboration in modern healthcare, and it is a model that will undoubtedly spread across other fields and continents in the coming years.
As we continue to lay the groundwork for this digital revolution, it is important to remember that every small improvement contributes to the larger goal of better, more responsive care. Through persistence, open dialogue, and a willingness to adapt, the healthcare community is well on its way to ushering in an era where digital tools and human compassion work hand in hand to create a more efficient, effective, and patient-focused system of care.
Originally Post From https://www.docwirenews.com/post/epros-and-the-future-of-cancer-care-real-world-lessons-from-oncopro
Read more about this topic at
Enhancing Oncology Model
Update: Enhancing Oncology Model Factsheet