Fascia Tympanoplasty: An In-Depth Look at Outcomes and Challenges
The world of ear surgery is filled with tricky parts and tangled issues, especially when it comes to repairing a perforated eardrum. In recent years, fascia tympanoplasty has become a common procedure to fix such problems, leading to improved hearing and anatomical restoration. Today, we take a closer look at the experience of one tertiary center, discussing how the procedure works, its outcomes, and the factors that may affect success. We aim to present a balanced editorial that highlights both the promising aspects and the nerve-racking challenges of the procedure.
Understanding Fascia Tympanoplasty
Fascia tympanoplasty involves the surgical repair of a perforated tympanic membrane using autologous connective tissue, typically taken from the temporal fascia. The technique is widely recognized for its accessibility and the biocompatible nature of the graft material. Its use not only helps restore the structure of the eardrum but also plays a critical role in improving hearing function. In this editorial, we will dive in to explore the procedure’s methodology, the fine points behind its success, and some of the hidden complexities that surgeons encounter.
How the Procedure Works
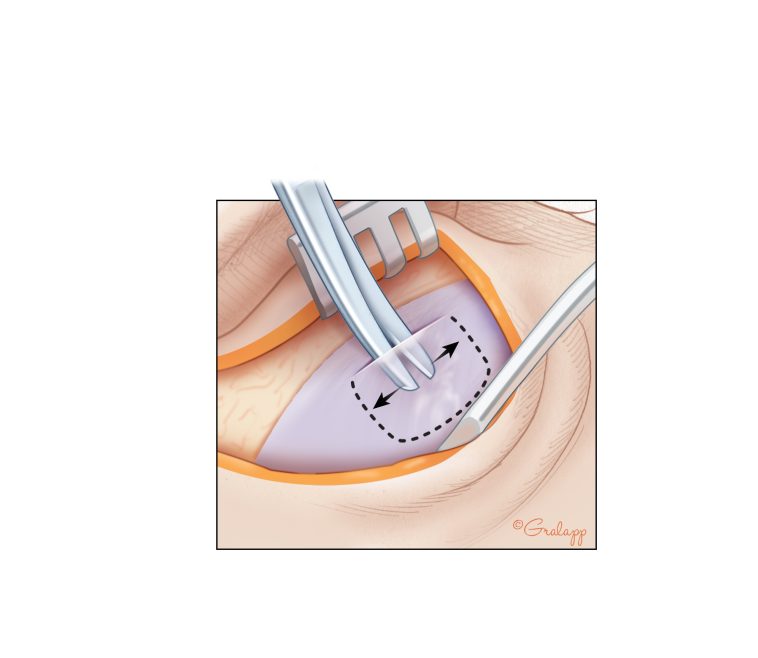
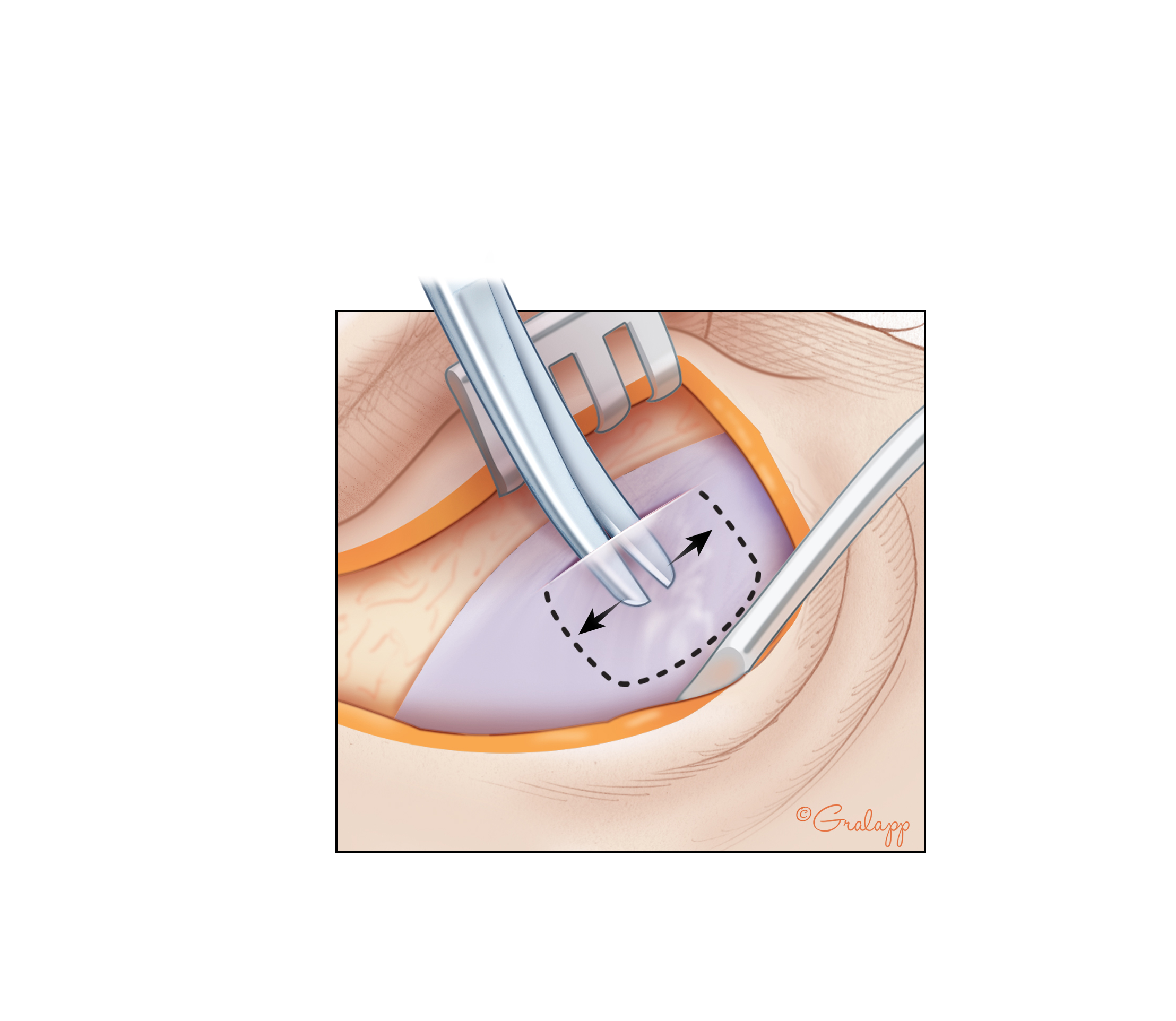
The surgery is designed to provide both anatomical and functional benefits. In simple terms, the surgeon places a piece of fascia over the perforation, allowing it to serve as a scaffold for healing. An intact and dry tympanic membrane within six months of the operation is considered an anatomical success, whereas hearing improvement—in terms of a reduced air-bone gap—is seen as a functional success.
Some key aspects of the procedure include:
- Harvesting the Graft: The temporal fascia, a readily available resource, is used because of its compatibility and ease of harvest.
- Placement Techniques: Surgeons may choose between underlay, overlay, or even a hybrid approach like over-under tympanoplasty to optimize outcomes for different perforation types.
- Surgical Refinements: Modern advancements, including endoscopic tympanoplasty, aim to reduce the overall operation time, minimize post-operative pain, and improve the surgical view of the middle ear.
Comparing Graft Materials: Autologous vs. Alloplastic Options
While the temporal fascia remains the favorite for many ear surgeons, there are alternatives available. Autologous grafts, including skin canal, conchal perichondrium, and cartilage, offer different strengths and weaknesses. Some studies suggest that cartilage might be preferable in cases where revision surgery is required, due to its durability and resistance to infections. However, alloplastic materials have been touted for faster healing and quicker recovery times, though these benefits are not always consistent in clinical practice.
In the midst of these options, the choice of graft material is a decision made on a case-by-case basis and depends heavily on the surgeon’s experience as well as the unique characteristics of the perforation.
Examining the Data: Surgical Outcomes and Patient Perspectives
The retrospective study from King Abdulaziz Medical City in Jeddah provides a wealth of insights into the successes and issues found in a real-world clinical setting. Over a period between 2017 and 2023, 71 fascia tympanoplasty procedures were carried out and the results were very promising overall. However, as with any surgical procedure, there were some nerve-racking twists and turns in the journey to recovery.
Outcomes: Anatomical and Functional Successes
The study reported an anatomical success rate of 83.1%—meaning that in the majority of cases, the graft took hold without further issues. Functionally, among the patients who underwent post-operative hearing assessments, about 57.9% showed improved hearing thresholds. This improvement was measured by comparing pre-operative and post-operative decibel levels, and the significant reduction in hearing gap is a clear indicator of functional benefit.
From the study, a few key observations stand out:
- The mean pre-operative decibel level was around 17.81 dB, which improved to a mean post-operative level of 8.96 dB.
- Residual or recurrent perforations were relatively uncommon, recorded in only 16.9% of cases.
- Post-operative complications, such as infection and wound problems, did exist, but most patients (62.3%) had no complications.
These numbers provide a clear indication that while the procedure is largely successful, every case has its own set of challenging and even confusing bits that need to be carefully managed.
Risk Factors and Influential Variables
When thinking about the predictors of surgical outcome, several factors come into play. The study highlighted age and the status of the graft as being significantly linked to how much the hearing improved. For example, younger patients and those whose graft completely healed often experienced better functional outcomes. This is likely due to the better regenerative capacity observed in younger individuals.
However, not all variables were shown to affect outcomes significantly. Factors such as gender, the presence of common comorbidities (like diabetes or hypertension), and even the size and location of the perforation did not have as much impact on the success of the surgery as once thought. The data adds to the continuing debate over which patient and perforation characteristics really influence surgical results. In the end, every surgeon must figure a path through these conflicting research findings to determine the best approach for each individual patient.
Detailed Breakdown of Pre-Operative and Post-Operative Parameters
Below is a simplified table summarizing some of the critical pre-operative and post-operative information observed in the study:
| Parameter | Details |
|---|---|
| Number of Procedures | 71 cases |
| Anatomical Success Rate | 83.1% |
| Hearing Improvement (Functional Success) | 57.9% (among assessed patients) |
| Pre-operative Decibel Level (average) | 17.81 dB |
| Post-operative Decibel Level (average) | 8.96 dB |
| Residual Perforation | 16.9% of cases |
| Complication Rate (any adverse event) | Approximately 38% experienced at least one complication |
This table should serve as a useful summary for those interested in the key performance indicators of the fascia tympanoplasty procedure.
Managing the Tricky Parts: Complications and Their Impact
No surgery is without its nerve-racking hurdles. In the case of fascia tympanoplasty, while the majority of patients have favorable outcomes, there are still instances of post-operative complications that must be addressed head-on. These complications range from infections to issues with wound healing, and although they often resolve with proper care, they do represent one of the more intimidating aspects for both patients and surgeons.
Common Post-Operative Complications
The study reported several types of complications:
- Infections: These included cellulitis, otitis externa, and otitis media in about 18.8% of patients.
- Wound Infections: Reported in roughly 5.6% of cases.
- Graft Failure: Seen in a small number of cases (approximately 5.8%), with some experiencing recurrence and others requiring revisions.
- Minor Otologic Symptoms: Such as pain, discomfort, and slight hearing loss.
The presence of complications, although not overly common, can be full of problems when they occur. It is critical to manage these issues promptly and effectively, so patients can recover without underscoring the overall effectiveness of the procedure.
Approaches to Minimizing Risks
Devising strategies to minimize complications is super important. To help improve outcomes, surgeons and healthcare teams should consider factors such as:
- Pre-Surgical Evaluation: A detailed review of the patient’s medical history, including any prior ear problems or systemic conditions, is essential.
- Infection Control Protocols: Rigorous adherence to sterile techniques during surgery and post-operative care routines helps reduce infection risks.
- Patient Education: Clear communication regarding what patients can expect — including potential complications — can help alleviate anxiety and ensure proper follow-up.
- Tailored Surgical Techniques: Adjusting the approach based on the size and location of the perforation,
as well as the patient’s individual needs, is key to achieving optimal outcomes.
Digging Into Patient-Centered Outcomes
While clinical data, statistics, and technical details are all critical, the patient’s experience and post-operative quality of life remain at the heart of any surgical success. For many, the challenge lies in finding their way through the confusing bits of pre-operative anxiety and post-operative recovery expectations.
Hearing Improvement and Daily Life
One of the most significant benefits of a successful fascia tympanoplasty is the improvement in hearing. Reduced decibel levels post-surgery mean that patients can enjoy better communication, improved safety in daily activities, and an overall enhanced quality of life. Even a seemingly small change in the air-bone gap contributes greatly to an individual’s confidence and ability to interact with their surroundings.
The study confirms that improved hearing is closely linked to the full anatomical closure of the tympanic membrane, pointing to the importance of achieving complete graft uptake. For patients, every dB of improvement can translate to a more vibrant and connected life.
Managing Expectations and Follow-Up Care
Managing your way through the post-operative phase involves regular monitoring, addressing any lingering issues, and following up on scheduled assessments. A few suggestions for patients include:
- Regular Audiological Assessments: These help in tracking improvements and guiding any additional therapy that might be needed.
- Clear Communication: Patients should have a clear channel of communication with their healthcare providers to discuss any concerns, especially if complications arise.
- Adherence to Care Plans: Following post-operative instructions diligently can reduce the risk of infections and other complications.
For healthcare providers, clear and compassionate communication before and after the procedure helps patients understand both the benefits and the potential issues — which can sometimes feel a bit overwhelming. It is a shared journey where both the patient and the medical team work together to secure the best possible outcome.
Weighing the Evidence: Balancing Promising Results with Challenges
The retrospective study offers insightful data that supports fascia tympanoplasty as a viable and largely successful method for repairing the perforated tympanic membrane. With an overall anatomical success rate exceeding 80% and notable improvements in hearing for a substantial number of patients, the procedure shows promise. Nevertheless, each case presents its own set of difficult twists and turns.
Pros and Cons as Seen in the Data
It helps to consider the pros and cons of the procedure to develop a well-rounded perspective:
- Pros:
- High anatomical success rates
- Meaningful improvements in hearing thresholds
- Low incidence of major complications
- Accessible autologous graft materials with excellent biocompatibility
- Cons:
- Residual perforations and graft failures occur in a minority of cases
- Some patients experience post-operative complications such as infections and pain
- There are still confusing bits regarding which prognostic factors most significantly affect outcomes
- The retrospective design of studies leaves some unanswered questions about long-term outcomes
Seeing both sides of the story allows clinicians and patients alike to work through the tricky parts and make informed decisions about the procedure. We must keep in mind that every surgical intervention carries some risk; however, the benefits of improved hearing and anatomical restoration often outweigh these challenges.
Expert Insights: What Does the Future Hold?
Looking ahead, the conversation around fascia tympanoplasty is not static. There are several areas where ongoing research and improved surgical techniques continue to shed light on the finer details of outcomes.
Optimizing Surgical Techniques
One area ripe for further exploration is how advancements in surgical techniques can help steer through the challenging twists and turns of the procedure. For instance, the integration of endoscopic approaches has been shown to provide a wider view of the middle ear, reduce operation times, and lessen post-operative discomfort. By adopting these newer methods, surgeons can aim to boost the success rates even further.
Moreover, the development of improved graft materials, both autologous and alloplastic, might allow for more tailored approaches. Future research may also help clarify which patient characteristics—like age or the exact perforation criteria—contribute most significantly to successful outcomes.
Personalized Medicine in Otolaryngology
There is a growing emphasis on personalized medicine, where treatment is tailored to the individual rather than a one-size-fits-all approach. In the case of fascia tympanoplasty, this means taking a closer look at each patient’s unique profile before deciding on the surgical technique or type of graft to use. Such approaches could include:
- Comprehensive Pre-Operative Assessments:
- Detailed audiological testing
- Assessment of middle ear anatomy via CT imaging
- Careful evaluation of coexisting conditions or prior ear issues
- Customized Surgical Plans:
- Choosing between underlay, overlay, or hybrid techniques
- Deciding on the best graft type for the individual patient
- Post-Operative Follow-Up:
- Regular check-ups to monitor healing and auditory improvement
- Timely interventions if complications arise
These advances will not only improve outcomes but also provide both patients and clinicians a clearer pathway through the otherwise confusing bits of the surgical process.
Addressing the Small Distinctions: The Role of Age, Graft Closure, and More
One of the most talked-about factors in tympanoplasty outcomes is the patient’s age. According to various studies, including the one from King Abdulaziz Medical City, age plays a critical role in hearing improvement post-surgery. Younger patients tend to experience better auditory recovery, possibly because their bodies are better able to heal and integrate the graft material.
Another small but essential detail is the complete closure of the perforation. The study highlights that when there isn’t any residual perforation, patients show a noticeable gain in hearing. These fine shades of difference in healing underscore the need for surgeons to pay very close attention to every step of the procedure.
Other factors like gender, the presence of underlying conditions (such as diabetes or hypertension), and even the precise size and location of the tympanic membrane perforation were not always as predictive of success as one might assume. This means that while these factors should be considered, they do not necessarily dictate the final outcome. Surgical experience and careful patient selection remain key elements in finding your way to consistent, positive results.
Looking at the Bigger Picture: The Impact of Research and Collaboration
Fascia tympanoplasty, while proven effective in many cases, has also driven a broader discussion within the otolaryngology community. Researchers and clinicians are actively comparing notes, sharing strategies, and collaborating across institutions to better understand which approaches yield the best results. This kind of partnership is essential for tackling the tangled issues associated with surgical outcomes and refining techniques over time.
Collaborative Research Efforts
One promising avenue is the growing body of multi-center studies and meta-analyses that aggregate data from various tertiary centers. Such research efforts help to mitigate the limitations of single-site, retrospective studies by offering a more comprehensive look at which factors are truly key. In doing so, they also provide a more accurate picture of success rates, complications, and patient satisfaction.
Collaboration among academic institutions and clinical centers leads to shared best practices, driving innovations in both surgical techniques and post-operative care. This cooperation, while loaded with its own set of challenges, represents a genuine move toward optimizing patient outcomes on a broader scale.
Educational Initiatives and Professional Development
Continuous education is super important for both established and emerging ear surgeons. Professional development programs, surgical workshops, and conferences offer valuable opportunities to get into the nitty-gritty details of the procedure and to understand how new techniques can overcome some of the intimidating hurdles of older methods.
For instance, many educational sessions now focus on how to:
- Adapt surgical techniques based on the unique anatomy of each patient
- Handle unexpected challenges during the surgery calmly and effectively
- Incorporate state-of-the-art endoscopic tools for better surgical visualization
- Extract maximal auditory benefit through precise graft placement and minimal tissue trauma
This kind of ongoing learning ensures that even as challenges arise, surgeons are well-prepared to figure a path through the maze of subtle details that influence outcomes.
Conclusion: Balancing Promise and Challenges in Fascia Tympanoplasty
In today’s discussion, we have taken a closer look at fascia tympanoplasty—a surgical solution designed to repair perforated tympanic membranes and improve hearing. The data from a tertiary center illustrates that while the procedure generally delivers high rates of anatomical success and meaningful improvements in hearing function, it is not without its tricky parts and nerve-racking challenges.
The procedure’s success is largely dependent on proper graft uptake and the ability to achieve a complete closure of the perforation. Younger patients and those without residual perforation tend to experience better auditory improvements. However, not all variables, such as gender or the exact size and location of the perforation, have been found to significantly impact results. This suggests that while certain factors play a key role, the overall outcome may depend more on the surgeon’s skill and careful post-operative care than on patient demographics alone.
Moreover, the discussion is far from black and white. There remain subtle parts and slight differences in findings across studies, highlighting the need for more robust, prospective research. Such studies would help to clarify which factors truly matter, steering clinical practice toward ever-improving outcomes.
From a patient’s perspective, the promise of improved hearing and a better quality of life offers a compelling reason to consider fascia tympanoplasty. Yet, it is crucial to be aware of both the benefits and the potential risks involved. Clear communication, thorough pre-operative evaluations, and vigilant post-operative care are all essential to ensuring the best possible experience for those undergoing the procedure.
Ultimately, fascia tympanoplasty stands as a testament to the innovations in ear surgery—a field where science and skill combine to overcome even the most intimidating surgical challenges. With ongoing collaborative research and educational initiatives, the twists and turns of this procedure are becoming less overwhelming, offering renewed hope and tangible benefits to patients around the globe.
As we continue to explore and refine surgical techniques, the otolaryngology community remains committed to improving patient outcomes. By shining a light on both the successes and the areas that still need work, we can navigate the complex yet promising landscape of fascia tympanoplasty. The journey may at times be loaded with issues, but it is ultimately one that leads to clearer hearing, better life quality, and a more confident future for countless patients.
Originally Post From https://www.cureus.com/articles/353536-fascia-tympanoplasty-a-tertiary-center-experience
Read more about this topic at
Tympanoplasty Outcomes: A Review of 789 Cases
Evaluation of Factors Affecting the Surgical Outcome in …