Refining Treatment Approaches in High-Risk Melanoma: A Closer Look
The latest updates from the 2025 ASCO Annual Meeting have certainly stirred conversation among oncology specialists and patients alike. While the meeting did not generate overwhelming practice-changing data, it offered several practice-affirming insights into the treatment of high-risk and advanced melanoma. In this opinion editorial, we take a closer look at the research presented, highlight the tricky parts of treatment design, and discuss what these findings mean for patients, families, and clinicians navigating this challenging field.
Understanding Single-Agent Immunotherapy Versus Combination Therapy
The ASCO 2025 meeting reinforced that for patients with stage 2 to 4 melanoma, the current standard of care remains anti-PD-1 monotherapy after surgical resection rather than switching to an intensive two-drug regimen. This reaffirmation is important because it simplifies treatment strategies for many patients who might otherwise face the overwhelming complexities of managing a combination therapy.
Dr. Vincent Ma, a respected voice in medical oncology at the University of Wisconsin School of Medicine and Public Health, explained that the data, especially from the RELATIVITY-098 study, did not favor the use of dual immunotherapy in the adjuvant setting. In his view, the fine points of the study reveal that the potential benefits of Opdivo (nivolumab) plus Opdualag (relatlimab) do not outweigh the additional challenges that come with a two-drug regimen. For patients and providers grappling with which option to pursue, this means the simpler, single-agent approach is still the key pathway.
This finding is significant because it helps steer treatment decisions away from complicated and potentially intimidating multi-drug treatments. Instead, it suggests that patients can continue with established, proven regimens that minimize the number of twists and turns encountered during their treatment journey.
Assessing the Duration of Immunotherapy: A Closer Look at the DANTE Trial
Another topic that sparked considerable debate at ASCO 2025 was the appropriate duration of immunotherapy for advanced melanoma. Currently, patients undergoing treatment for advanced-stage melanoma typically receive a minimum of two years of immunotherapy. However, there is an increasing curiosity to determine if one year of treatment might be sufficient, reducing the nerve-racking burden of long-term therapy.
The DANTE trial was designed to poke around this very question. By examining whether a shorter, one-year treatment course would be non-inferior to the traditional two-year regimen, the study aimed to address a question that many patients and providers face:
- Is the full two-year schedule necessary for the benefits seen in clinical trials?
- Can early responses to treatment allow for a shorter duration of therapy?
- How might reducing treatment duration affect the overall progression-free survival?
The trial, conducted mainly in the United Kingdom, enrolled only a small fraction of the planned 1,200 patients (with 166 ultimately enrolled), making the study underpowered. Despite the reduced patient number, preliminary data suggested that one year of immunotherapy was not statistically inferior to the two-year course in terms of progression-free survival. Nevertheless, due to the underpowered nature of the study, the standard recommendation continues to be a minimum of two years of immunotherapy for advanced melanoma.
In essence, while the study introduces the possibility of reducing treatment duration, it also underscores the importance of caution. Without robust statistical confirmation, the findings serve as an impetus for future studies rather than an immediate overhaul of current clinical practice. Patients should thus be advised that, for now, sticking with the standard two-year regimen remains the super important guideline.
Delving Into Adjuvant Therapy Updates: Insights from the RELATIVITY-098 Trial
The RELATIVITY-098 trial was another focal point of discussion at the meeting. This study sought to determine whether the combination of Opdivo and Opdualag could enhance recurrence-free survival when used as adjuvant therapy after complete surgical resection for stage 3 or stage 4 melanoma.
Historically, two main strategies exist for treating resected high-risk melanoma: anti-PD-1 monotherapy (using drugs like Opdivo or Keytruda) and, in cases where a patient has a BRAF V600 mutation, BRAF/MEK targeted therapy. Although both strategies have been shown to reduce the risk of recurrence, not all patients achieve the same level of benefit. In theory, adding a second drug might improve outcomes, but the RELATIVITY-098 trial revealed that for patients with surgically treated stage 3 or 4 melanoma, the addition of Opdualag did not offer an appreciable improvement over single-agent anti-PD-1 therapy.
These findings emphasize that, despite some promising data in unresectable settings, the extra layer of complexity introduced by a two-drug approach in the adjuvant situation does not necessarily translate to improved efficacy. This insight is crucial because it simplifies treatment decisions and helps avoid the additional side effects and management challenges that can accompany combination regimens. As Dr. Ma pointed out, there was no specific subset of patients who seemed to benefit more from the two-drug approach, which further avers that the single-agent strategy should remain the mainstay.
Essential Considerations for Patients and Providers
It is important to recognize that clinical trial data, while very informative, also come with their own set of tricky parts and tangled issues. For instance, even though studies like DANTE and RELATIVITY-098 have provided valuable insights, they also remind us of the significant challenges involved in trial design and patient enrollment. Here are some key aspects healthcare professionals and patients should consider:
- Study Power and Enrollment: A small sample size can lead to underpowered studies, which might not provide a comprehensive view of the treatment’s effectiveness. This highlights the nerve-racking reality of clinical trial limitations.
- Recurrence-Free Survival vs. Overall Survival: While progression-free or recurrence-free survival is an important marker, the ultimate goal is to improve overall survival. The current studies did not fully shed light on this, leaving room for future investigation.
- Side-Effect Management: Combination therapies often introduce more side effects. Maintaining a focus on treatments with fewer additional risks is a key consideration, especially given the overwhelming personal and social implications of side effects.
- Quality of Life: The length and intensity of treatment can have a significant impact on a patient’s day-to-day life. Both one-year and two-year therapy regimens need to be balanced against factors such as work, family responsibilities, and the overall well-being of the patient.
These factors underscore the irony of how simpler, well-established protocols often end up being more advantageous than potentially more aggressive, yet complicated, treatment plans. For many patients, having a straightforward treatment regimen without the confusing bits of additional drugs can lead to a smoother, more manageable journey through their recovery.
Weighing the Pros and Cons: Immunotherapy Duration and Side Effects
One intriguing aspect of these studies is the balance between treatment duration and the side-effect burden. On one hand, patients with advanced melanoma face the daunting prospect of a two-year immunotherapy course—an intimidating commitment that can be both physically and emotionally overwhelming. On the other hand, shorter treatments could potentially reduce treatment-related morbidity, side effects, and the toll these regimens take on daily life.
Below is a table summarizing the key pros and cons associated with two-year immunotherapy versus a potential one-year regimen based on current evidence:
| Treatment Duration | Pros | Cons |
|---|---|---|
| Two-Year Course |
|
|
| One-Year Regimen |
|
|
This side-by-side comparison illustrates that while shortcuts in treatment duration sound appealing, the existing evidence supports caution—even if, on first glance, the idea of a shorter regimen seems like an attractive way to reduce the overwhelming commitment of extending treatment schedules.
Future Directions in Melanoma Research: What Lies Ahead?
The studies presented at ASCO 2025 are a snapshot of a dynamic, evolving field. There are several ongoing efforts aimed at reducing the burdens of treatment while ensuring that patient outcomes are not compromised. Here are a few areas where upcoming research may shine a light on less intimidating possibilities:
Personalized Treatment Based on Early Response
Future studies are expected to assess whether treatment duration can be dynamically adjusted based on the individual patient’s early response to immunotherapy. By taking a closer look at early biomarkers and treatment responses, clinicians hope to determine if patients who respond quickly could safely receive a shorter duration of therapy. Such dynamic treatment plans could allow patients to experience fewer side effects without compromising overall survival outcomes.
Combination Therapies: Finding the Right Balance
While the dual-drug approach in the adjuvant setting did not demonstrate additional benefits over monotherapy in the RELATIVITY-098 trial, research is ongoing to find the right balance when combining immunotherapies. This involves not only understanding which patients might benefit, but also carefully evaluating the fine details of drug dose and scheduling. The aim is to minimize the additional risk of side effects while maximizing any potential improvements in efficacy.
Quality of Life and Survivorship Studies
Beyond survival metrics, quality-of-life studies are emerging as a key focus. These studies are loaded with issues related to the hidden complexities of long-term treatment side effects, psychological well-being, and the economic burdens associated with prolonged treatments. Managing the patient experience throughout the treatment journey is as critical as measuring clinical outcomes. Future research that combines clinical efficacy with patient-reported outcomes will help both patients and providers figure a path through the maze of treatment options.
Technological Advances in Monitoring and Drug Delivery
Advancements in digital health tools and monitoring technologies are also on the horizon. Innovations such as remote monitoring, telemedicine consultations, and precision medicine tools are all trying to simplify the twists and turns of cancer treatment, allowing for earlier detection of side effects, more personalized dosing, and better overall management of the patient journey.
Insights for Clinicians: Managing the Path Forward
For healthcare providers, the data from ASCO 2025 offers both reassurance and new challenges. In practical terms, here are some strategies to help steer through the tricky parts of melanoma treatment based on current evidence:
- Maintain the Established Standard: Continue to utilize anti-PD-1 monotherapy as the primary adjuvant treatment following resection in stages 2, 3, or 4 melanoma until further robust evidence supports a change.
- Monitor Emerging Data: Keep a close watch on new studies addressing treatment duration and combination therapy. This is a field driven by rapid advancements, and early identification of promising research can help refine treatment protocols sooner.
- Emphasize Patient-Centered Care: Discuss treatment plans thoroughly with patients, considering the subtle details of side-effect profiles, quality-of-life impacts, and personal lifestyle considerations. Listening to patient preferences is as key as understanding the scientific data.
- Encourage Participation in Clinical Trials: Recognize that now is a pivotal time for research. Whenever appropriate, referring patients to clinical trials can contribute to the collective understanding about optimal treatment regimens while offering patients access to potential new therapies.
This practical guidance not only underscores the essential aspects of current care but also offers a framework for managing future adjustments as new research emerges.
Patient Perspectives: Taking a Closer Look at the Treatment Journey
From the patient’s viewpoint, the road to recovery through melanoma treatment can be full of confusing bits and overwhelming challenges. Treatment regimens that are excessively complex or lengthy can contribute to a sense of being lost in a maze of appointments and side effects. Here are a few patient-centered aspects that deserve attention:
- Psychological Impact: Long-term therapy has a significant psychological burden. Patients have to cope with not only the physical side effects but also the constant reminder of their diagnosis. A potentially shortened treatment course might ease some of this pressure.
- Practical Considerations: The frequency of treatment—often every three to four weeks during immunotherapy—can disrupt daily routines and work commitments. The possibility of a shorter regimen could provide much-needed relief and allow patients to get around their daily responsibilities with a little less stress.
- Financial Factors: Beyond the physical and emotional challenges, the financial strain cannot be overlooked. Frequent treatments contribute to higher costs and more time off work, which further adds to the overall stress of managing the disease.
For many individuals facing advanced melanoma, the promise of a simpler, proven treatment regimen is not just a clinical matter, but a matter of daily survival. As clinicians and researchers work together to uncover the fine shades of treatment efficacy and safety, the ultimate aim is to make the journey as manageable as possible for those involved.
Bridging the Gap Between Research and Real-World Practice
Even though clinical trials like those discussed at ASCO often generate headlines and discussion within the medical community, applying these findings in everyday practice involves negotiating several practical challenges. The following bullet points outline some of the basic steps needed to bridge the gap between interesting trial data and real-world application:
- Implementing standardized treatment protocols that are easy to follow.
- Educating healthcare teams on the subtle details of newly released study outcomes.
- Ensuring open channels of communication so that patients understand their options.
- Monitoring patient outcomes closely to confirm that trial results are replicable in community settings.
By focusing on these actionable steps, the clinical community can take advantage of both established treatments and emerging research, ensuring that the care provided reflects the current best practice while remaining flexible enough to adapt as new insights become available.
Examining the Broader Landscape of Melanoma Treatment
In today’s rapidly evolving oncology environment, the treatment of melanoma is affected by multiple factors. From managing the fine points of treatment regimens to addressing the hidden complexities of patient responses, the conversation is loaded with challenges that are both clinical and personal. Some additional factors to consider include:
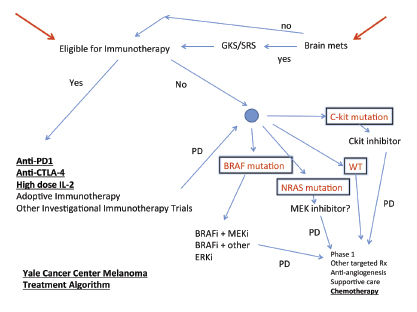
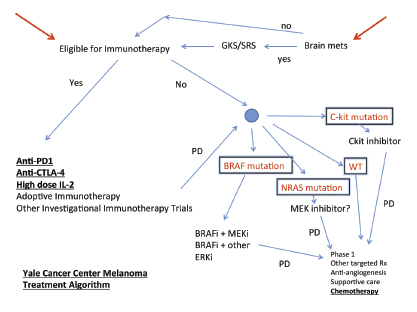
- The Role of Genetic Mutations: For patients with a BRAF V600 mutation, targeted therapies remain an essential component, offering an alternative approach to those who are not ideal candidates for immunotherapy alone.
- The Importance of Multidisciplinary Teams: Successful melanoma treatment rarely depends on a single modality. Instead, collaboration among oncologists, dermatologists, surgeons, and supportive care teams is super important to manage both the treatment and its side effects effectively.
- Access to Care: Socioeconomic factors and geographic location are sometimes overlooked but are crucial in ensuring that patients receive timely, high-quality care. Efforts to increase access and streamline care are fundamental in managing this disease.
These factors underscore the complexity of treating melanoma, where every decision must take into account both the clinical evidence and the individual circumstances of patients. Simplifying treatment approaches where possible—while still aiming for the best outcomes—remains a guiding principle throughout many of these discussions.
Future Research Priorities: Navigating the Next Steps
Looking ahead, the field of melanoma treatment is poised for continued evolution. Researchers and clinicians are committed to exploring numerous avenues that could potentially lead to breakthroughs not just in survival, but in quality of life as well. Some of the most promising areas of upcoming research include:
- Biomarker-Driven Therapy: Identifying early response markers will be crucial in determining which patients can safely receive shortened treatment. This research is super important because it shifts the approach from a one-size-fits-all methodology to personalized care.
- Combination Versus Monotherapy Studies: Further studies are needed to parse out the fine shades of benefit between combining drugs versus sticking with a single-agent approach, particularly to determine if there are specific patient subgroups that could indeed benefit from a dual-drug regimen.
- Quality of Life Metrics: As mentioned earlier, future trials will increasingly include patient-reported outcomes to assess not only clinical efficacy but also the impact on daily living. These outcomes are essential for making informed decisions about treatment duration and intensity.
- Innovative Drug Delivery Mechanisms: New methods of delivering drugs that reduce side effects and improve patient compliance are on the horizon. Research in this sector could revolutionize how therapy is administered, making treatment less invasive and more convenient.
Through continued investigation and collaboration, the oncology community is committed to untangling the multiple layers of these treatment strategies. While current data reaffirm the importance of anti-PD-1 monotherapy following resection, the quest for optimized, patient-friendly approaches to melanoma care is far from over.
Conclusion: Balancing Evidence, Safety, and Patient Experience
The ASCO 2025 updates on high-risk melanoma treatment present a complex picture. On one level, the reaffirmation of anti-PD-1 monotherapy after resection offers comfort to those managing the disease, providing a clear and familiar pathway amidst the numerous twists and turns of cancer treatment.
At the same time, studies like the DANTE trial and the RELATIVITY-098 trial invite all stakeholders to question whether there are opportunities to simplify the treatment process—be it by shortening the duration of immunotherapy or by rethinking the need for combination approaches. The evidence thus far, while promising in certain respects, is not yet sufficient to radically alter current protocols.
For patients, the reassurance that current treatment standards are still backed by robust data is a key takeaway. At the same time, the potential for future changes that might reduce the burden of therapy offers hope. This dual message emphasizes that it is essential to keep abreast of emerging research while maintaining established, proven treatment pathways.
Clinicians are encouraged to find their way through these challenging decisions by focusing on patient-centered outcomes. This means weighing not only the clinical benefits but also the subtle details of how treatment regimens impact quality of life. As research continues to evolve, a collaborative approach—where patients, caregivers, and healthcare providers work together—will be critical in managing the tangled issues of melanoma care.
Ultimately, the key to navigating the future of melanoma treatment is flexibility combined with a commitment to evidence-based practice. The current standard of care remains deeply rooted in the data we have, but ongoing studies may one day illuminate a clearer, less intimidating path forward. Until then, the combined efforts of the oncology research community, clinicians, and patients will continue to drive improvements in how we manage this challenging disease.
As we look to the future, the integration of real-world patient experiences with rigorous clinical research will be super important. Only by addressing both the scientific and human aspects of treatment can we truly hope to improve outcomes in a way that balances survival with quality of life. This is the path forward—a journey that, while full of confusing bits and nerve-racking challenges, holds the promise of a brighter and less complicated future for melanoma patients.
In conclusion, while the ASCO 2025 meeting did not usher in a new standard immediately, it reinforced the necessity of balancing proven treatment efficacy with the practical demands of patient care. It is a reminder that in the intricate realm of oncology, sometimes the best path forward is to rely on established protocols while continuing to explore and refine them for a future where treatments are both effective and easier for patients to manage.
Originally Post From https://www.curetoday.com/view/refining-treatment-approaches-and-advancements-in-high-risk-melanoma
Read more about this topic at
Refining Treatment Approaches and Advancements in …
Different Treatment Options for Melanoma Skin Cancer