Escherichia coli Cellulitis in Immunocompromised Patients: A Hidden Challenge in Modern Healthcare
The realm of infectious diseases is filled with tricky parts and subtle details that can complicate even the most straightforward cases. In recent years, clinicians have been increasingly confronted with unusual pathogens causing skin infections, particularly among those who are immunocompromised. One such case involves Escherichia coli cellulitis—a condition that, while rare, forces healthcare providers to figure a path through a maze of diagnostic uncertainties and treatment decisions. This editorial is an opinion piece that examines the case of a 79‐year‐old woman with Waldenström macroglobulinaemia and AL amyloidosis, and it explores the broader implications of managing atypical infections in high‐risk patients.
At the heart of this discussion lies the challenge of handling infections when the standard approach does not yield the expected results. When conventional antibiotics prove ineffective and cultures reveal unconventional organisms, medical teams are compelled to take a closer look and adjust their strategies accordingly. The following sections will dig into the diagnostic journey, the treatment dilemmas, and the lessons learned, all while using a neutral tone that appreciates the complexities involved in modern medicine.
Understanding Escherichia coli and its Unexpected Role in Skin Infections
Traditionally, when doctors think of skin infections like cellulitis, they imagine bacteria such as Staphylococcus aureus or Streptococcus species. Escherichia coli—a normally gut-dwelling bacterium—rarely comes into the picture as a skin pathogen. However, as reported in our case of a 79-year-old patient, E. coli can indeed be the culprit, especially in individuals with a compromised immune system.
There are several reasons why E. coli might appear in settings where it is least expected:
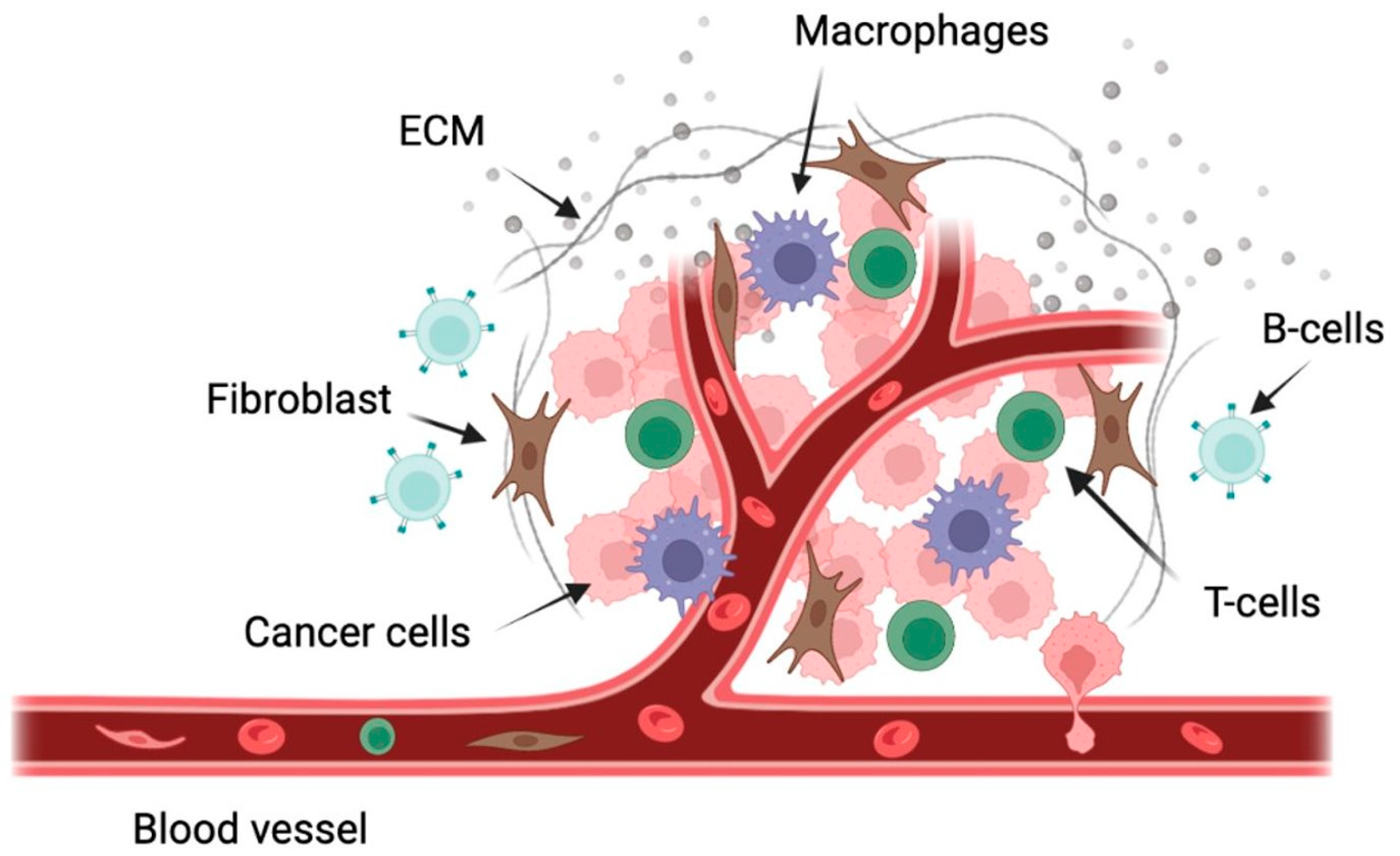
- Immune System Weakness: Patients undergoing chemotherapy, or those with haematological malignancies, are more vulnerable to infections from bacteria not commonly associated with skin diseases.
- Antibiotic Pressure: Frequent use of empirical antibiotics can change the local bacterial flora at infection sites, paving the way for more unusual organisms to establish an infection.
- Underlying Comorbidities: Conditions such as chronic kidney disease or AL amyloidosis can further complicate the infection landscape and compromise the host defense mechanisms.
When faced with such a scenario, clinicians are forced to steer through a tangled maze of potential culprits and treatment pathways. This case serves as a reminder that the microbial world is full of surprises, and that pathogens once thought to be confined to one area of the body can sometimes appear in unexpected places.
Diagnosing Unusual Pathogens: The Tricky Parts of the Process
One of the most intimidating aspects of managing infections in immunocompromised patients is pinpointing the atypical organism responsible for the illness. In our case, the patient’s initial treatment with flucloxacillin—a standard therapy for cellulitis—did not yield the improvement expected. This lack of improvement raised red flags, prompting the medical team to get into further investigations.
Diagnosing E. coli cellulitis involves several challenging steps:
- Clinical Recognition: Recognizing that an infection is not responding to standard treatment is the first sign that the underlying organism might be unusual.
- Blood Cultures: Identifying E. coli in blood cultures redirected the diagnostic focus. However, because positive cultures necessitate ruling out other infection sources, the process becomes even more nerve-racking.
- Imaging Studies: Radiological investigations such as computed tomography (CT) scans and Doppler ultrasounds become crucial to exclude other sources of infection—like intra-abdominal, biliary, or deep soft tissue abscesses.
The diagnostic process is often loaded with little twists and turns. When blood tests show signs of infection but the primary site is ambiguous, clinicians must figure a path through a series of tests to get a complete picture. This systematic approach is essential, as it prevents misdiagnosis and ensures that patients receive the appropriate help quickly.
The Overwhelming Journey of Excluding Alternative Infection Sources
When lab results reveal the presence of E. coli in the context of cellulitis, the immediate reaction is to confirm whether the skin infection is truly primary, or if there is an underlying, perhaps hidden, source that needs attention. In our patient’s case, several additional investigations were performed:
- CT Imaging: A CT scan of the abdomen and pelvis provided a thorough look into deep-seated collections. Despite the nerve-racking wait for results, the scan ruled out any major intra-abdominal sources such as biliary infection or perinephric collections.
- Doppler Ultrasound: This was used to exclude the possibility of deep vein thrombosis—a condition that could mimic or even exacerbate skin infections.
- Urine Analysis: Ruling out urinary sources of infection was equally important. Urine microscopy and culture did not yield any E. coli growth, further pointing the finger at the skin as the primary focus.
Each of these diagnostic steps contributes to unraveling the confusing bits of the overall picture. They exemplify the importance of ruling out other causes, thereby ensuring that the therapeutic focus remains on the correct pathogen. The ability to work through these intertwined investigations is a testament to modern medicine’s diagnostic acumen.
Treatment Dilemmas: Combining Antimicrobials to Tackle Atypical Pathogens
Once E. coli was confirmed as the pathogen in the bloodstream, the treatment approach had to be reassessed. The traditional antibiotics for cellulitis, such as flucloxacillin, did not effectively address the infection. This scenario led clinicians to adjust their treatment strategy and combine different antibiotics.
Key considerations in designing the treatment plan included:
- Antibiotic Sensitivity: Laboratory tests revealed that the E. coli strain was resistant to commonly used antibiotics, including ciprofloxacin and co-trimoxazole, but remained sensitive to alternatives like co-amoxiclav.
- Combination Therapy: The patient was initially treated with intravenous co-amoxiclav, followed by an additional course of oral flucloxacillin to help manage persisting symptoms, particularly the swelling and pain in the infected area.
- Tailored Duration: The length of therapy was adjusted based on both clinical improvement and lab markers. This flexible approach allowed clinicians to carefully steer through the process and customize therapy to the patient’s needs.
If we list the treatment components, they could be organized as follows:
| Treatment Modality | Description |
|---|---|
| Intravenous Co-amoxiclav | Used as initial therapy, administered three times per day to combat the bloodstream infection. |
| Oral Flucloxacillin | Added later to target persistent local symptoms of cellulitis, with dosing of 1 gram four times per day. |
| Antibiotic Sensitivity Testing | Guided the antibiotic choice, ensuring the selected regimen was effective against the identified E. coli strain. |
This multi-pronged approach to therapy demonstrates that when unexpected challenges arise, blending different treatment modalities can be the key to overcoming complications. The ultimate goal is always to ensure that the patient recovers with minimal residual issues, especially when the infection initially appears to be off-track.
Lessons from the Case: Fine Points in Managing Immunocompromised Patients
The case of the 79-year-old woman provides several super important takeaways that are applicable to managing infections in high-risk populations. Here are a few fine points that clinicians should consider:
- Early Recognition and Flexibility: Prompt recognition that a patient is not responding to standard therapy can be the first clue that something atypical is at play. Being flexible with diagnostic strategies, such as ordering blood cultures early, can save precious time in critical situations.
- Comprehensive Evaluation: Examining all possible infection sources is a tricky part of the process. Even when blood cultures show E. coli, clinicians must rule out other potential origins by performing advanced imaging and additional lab tests.
- Customizing Treatment Plans: There is no one-size-fits-all approach. The combination of intravenous and oral therapies tailored to the individual’s response illustrates the need to adapt treatment strategies, a point that must not be overlooked when dealing with atypical pathogens.
- Antibiotic Stewardship: Ensuring appropriate use of antibiotics is super important in preventing the emergence of resistant strains. This case highlights the necessity of grounding therapy decisions in robust microbiological data.
For medical professionals, these lessons translate into a need to stay alert for any small distinctions that might signal a deeper problem. It is crucial to be proactive and thorough in testing when dealing with patients who have underlying conditions that dampen their immune responses.
Digging into the Impact of Multidrug-Resistant E. coli on Healthcare Systems
The emergence and spread of multidrug-resistant E. coli have significant implications for healthcare systems worldwide. When organisms become resistant to therapies that were once effective, the twists and turns of treatment become even more challenging. The following points highlight some of the key issues:
- Increased Hospital Stays: Infections caused by resistant strains often result in longer hospital admissions due to the need for more intensive therapy and careful monitoring.
- Higher Mortality Rates: As resistance grows, the risk of life-threatening complications escalates. This makes early diagnosis and effective treatment strategies critical for patient survival.
- Economic Impact: Longer treatments and the use of more expensive antibiotic regimens can place a strain on healthcare budgets. Hospitals must balance the cost of newer therapies against the benefits they provide in combating resistant infections.
Healthcare providers must figure a path through these economic and clinical challenges. There is a collective responsibility to invest in research and adopt new techniques for managing such infections. This means supporting robust surveillance systems, encouraging prudent antibiotic use, and fostering collaboration between microbiologists, infectious disease specialists, and frontline clinicians.
Working Through Resource Challenges and Patient Outcomes
Clinicians often face resource-based challenges when managing unexpected pathogens. The diagnosis and subsequent treatment of E. coli cellulitis in an immunocompromised patient is a perfect example of where limited resources, combined with a need for prompt action, can make the situation even more tense. Several key issues arise:
- Access to Advanced Diagnostics: Not every medical facility has immediate access to comprehensive imaging tools or advanced laboratory testing. In such cases, referring patients to higher-level centers becomes necessary.
- Expert Consultation: The involvement of specialists, such as microbiologists, can be key to piecing together the fine shades of the infection’s origin. Their insights help guide treatment options that might not be immediately apparent.
- Timely Decision-making: When clinicians are forced to get around limited resources, making swift yet informed decisions about therapy is essential. This balancing act is critical, as delays may lead to worsening of the patient’s condition.
In situations where standard protocols fall short, healthcare teams must work together, closely monitoring the patient’s response and remaining alert to any subtle signs of either improvement or deterioration. Ultimately, the objective is to deliver individualized care that not only addresses the infection but also supports the overall wellbeing of the patient.
Alternative Approaches and the Importance of a Multi-Disciplinary Team
Dealing with rare infections like E. coli cellulitis requires a team effort. The case under discussion reflects how a multi-disciplinary approach—combining the expertise of infectious disease specialists, radiologists, clinical microbiologists, and even pharmacists—is essential to achieve a positive outcome.
Consider the following benefits of engaging a multi-disciplinary team:
- Collective Expertise: When different professionals contribute their unique insights, the team is better equipped to make sense of the confusing bits and tangled issues associated with atypical infections.
- Consensus-Driven Decisions: Collaborative decision-making ensures that the chosen therapeutic approaches are built on a foundation of thorough discussion and shared experiences, which is particularly critical when dealing with rare or off-track pathogens.
- Enhanced Patient Support: Multi-disciplinary input provides a more comprehensive care plan, addressing both clinical and psychosocial aspects, which is especially important for vulnerable patients with multiple comorbidities.
This kind of collaborative approach can be the difference between a prolonged, complicated hospital stay and a smoother recovery pathway. While it may require extra coordination and communication efforts, the benefits for patient outcomes are undeniable.
Finding Your Way Through Antibiotic Stewardship and Modern Medicine
One of the most critical challenges facing modern medicine is the rising prevalence of antibiotic-resistant bacteria. The case of E. coli cellulitis in our immunocompromised patient serves as a stark reminder of why antibiotic stewardship must remain a key focus for health systems worldwide.
Key aspects of antibiotic stewardship include:
- Targeted Therapy: The decision to treat the patient with co-amoxiclav based on sensitivity testing instead of sticking to the usual empirical approach reflects a delicate balancing act that must be managed to reduce antibiotic resistance.
- Regular Monitoring: Keeping a close eye on clinical markers such as C-reactive protein (CRP) levels, white blood cell counts, and kidney function parameters is an invaluable tool to guide therapeutic adjustments during the treatment course.
- Education and Training: Continuous professional development ensures that medical teams are aware of the latest developments in antibiotic resistance and are prepared to apply new guidelines effectively.
Antibiotic stewardship is not simply about restricting the use of certain drugs; it encompasses the entire treatment process—from diagnosis to follow-up. It requires healthcare providers to remain vigilant and to be prepared to change tactics when small distinctions in laboratory results or patient responses hint at a need for a different approach. Ultimately, responsible antibiotic use is a must-have strategy for preserving the efficacy of current therapies and ensuring better outcomes for patients across the board.
Patient-Centered Care and the Role of Follow-Up
In a case as loaded with issues as E. coli cellulitis, patient-centered care remains at the forefront of the treatment journey. Even though the clinical discussions often focus on microbial patterns and treatment regimens, it is essential to remember that patient wellbeing is the primary goal. In this case, continual monitoring and follow-up played a key role in ensuring recovery.
Several measures help in providing compassionate, patient-centered care:
- Frequent Reassessment: Regular monitoring of clinical and laboratory markers allows physicians to adjust treatments and ensure that the patient’s condition is steadily improving.
- Clear Communication: Keeping the patient informed about their condition, the reasoning behind each treatment decision, and the expected progress helps ease the overwhelming aspects of the experience.
- Support Networks: Engagement with family members and caregivers can provide the necessary support system, which is especially critical when patients are navigating the twists and turns of a severe infection.
This holistic approach not only addresses the medical needs of the patient but also eases the emotional burden associated with managing a serious infection. In the end, the best outcomes are often achieved when clinical expertise is combined with empathetic, patient-focused care.
Healthcare Policy and the Future of Managing Complex Infections
The challenges posed by infections such as E. coli cellulitis have important implications not just on an individual level, but also for healthcare policy and practice. As our population ages and the number of immunocompromised patients increases, clinicians and policymakers must work together to ensure that health systems are equipped to manage such cases effectively.
Key future considerations include:
- Investment in Diagnostics: Funding advanced diagnostic tools and training healthcare personnel to interpret complex results can make a big difference in early detection and appropriate management of atypical infections.
- Research into New Therapies: Ongoing research into novel antimicrobial agents and alternative treatment strategies is super important in keeping pace with the evolving threat of antibiotic resistance.
- Policy Reforms: Developing streamlined guidelines and protocols for managing unusual infections, especially in immunocompromised individuals, can help standardize care and improve patient outcomes on a broader scale.
In addressing these areas, healthcare systems can better prepare for the challenging future ahead. Policymakers and clinical leaders must work hand in hand to create systems that can quickly adapt to the changing microbial environment, enabling clinicians to work through confusing bits and little details with confidence and clarity.
Final Thoughts: Embracing a Collaborative and Adaptable Approach in Medical Practice
The case of E. coli cellulitis in a patient with Waldenström macroglobulinaemia offers a striking example of the obstacles that can arise when the unexpected occurs. Despite the nerve-racking uncertainty at the outset, the patient’s treatment course demonstrated that with a flexible, team-based, and patient-centered approach, even rare and challenging infections can be managed successfully.
From the initial missteps with standard therapy to the eventual tailored treatment that combined intravenous co-amoxiclav with oral flucloxacillin, the journey underscores several key messages for modern medicine:
- Never Assume the Usual Suspects: When a patient is not responding as expected, it is crucial to dig into alternative possibilities and rule out secondary sources.
- Teamwork is Essential: Effective collaboration between various specialists can help sort out the tangled issues that arise, paving the way for more precise and effective treatments.
- Adaptability Saves Lives: The ability to modify treatment plans based on up-to-date microbiological data and clinical observations cannot be overstated. In cases like these, being willing to change direction is not merely beneficial—it is a key element in achieving a positive outcome.
- Focus on the Patient: Beyond the science of microbiology and pharmacology is the human side of medicine. Ensuring that patients are kept informed and supported throughout their journey is as critical as any diagnostic or therapeutic intervention.
This case should serve as a wake-up call to healthcare providers everywhere, reminding them that infections are rarely straightforward and that each case may come with its own set of twists and turns. By staying alert, working collaboratively, and maintaining a commitment to antibiotic stewardship, the modern medical community can effectively manage these challenging cases and ultimately improve patient outcomes.
As we think about the future, it is clear that rare infections like E. coli cellulitis are part of a broader shift in the infectious disease landscape. These occurrences challenge us to update our diagnostic tools, rethink our treatment strategies, and advocate for better resource allocation to support comprehensive care. Although the path is often loaded with problems and complicated pieces, the pursuit of excellence in healthcare demands that we tackle these challenges head-on.
In conclusion, dealing with unusual bacterial infections requires a dynamic, adaptive, and empathetic approach. The fine points of diagnosing and treating such conditions—not just in immunocompromised patients but across all populations—highlight how modern medicine continues to evolve in response to emerging microbial threats. The lessons learnt from this case, combined with ongoing research and policy development, can help guide clinicians as they work through the unpredictable and often intimidating world of infectious diseases.
We must always be prepared to re-examine our assumptions and tailor our treatments to each patient’s unique context. By doing so, we honor the principle that every patient deserves the best possible care—a care system that is as flexible, resilient, and innovative as the challenges it faces.
This editorial is a call to action for all healthcare professionals: embrace change, collaborate closely, and always be on the lookout for those subtle details that can make all the difference between a prolonged hospital stay and a swift recovery. In the end, successfully managing infections like E. coli cellulitis is not just about eradicating a pathogen, but about ensuring that our healthcare systems evolve in step with the ever-changing landscape of microbial threats.
Ultimately, the medical community must continue to invest in research, education, and policy reforms that support diagnostic precision and targeted therapies. Each case, no matter how rare, contributes valuable insights into the art and science of medicine. With every challenge that we overcome, we get one step closer to a healthcare system that is better equipped to tackle the nervous, overwhelming twists and turns of modern infectious diseases.
As we move forward, let this case serve as a reminder that unconventional infections require unconventional solutions—ones that are grounded in scientific evidence, driven by a spirit of collaboration, and aimed at achieving the best outcomes for patients, regardless of the complexity of their condition.
In the dynamic interplay between emerging bacterial threats and cutting-edge medical practice, the key to success lies in our ability to stay ahead of the curve, to continuously learn, and to adjust our strategies as new data emerge. With each patient encounter, every diagnostic test, and all treatment adaptations, the medical community is better prepared to face the challenges of tomorrow with confidence and determination.
Originally Post From https://www.cureus.com/articles/379336-escherichia-coli-cellulitis-in-a-patient-with-waldenstrm-macroglobulinaemia-a-case-report
Read more about this topic at
An unusual case of Escherichia coli cellulitis and …
Escherichia Coli bacteremia and rapidly progressive …