Revisiting HbA1c Reliability When Thalassemia Trait Enters the Picture
The case of a 46-year-old man with newly diagnosed diabetes mellitus and beta-thalassemia trait challenges the common assumption that hemoglobin A1c (HbA1c) is always a super important, must-have tool for tracking long-term glycemic control. In this opinion editorial, we take a closer look at the tricky parts of using HbA1c in patients with hemoglobinopathies and propose alternative, more reliable approaches to monitoring blood sugar. This discussion is particularly essential in regions where thalassemia traits are widespread, revealing the tangled issues that come up when established diagnostic methods and unexpected laboratory results collide.
When Standard Diabetes Assessment Gets Confusing
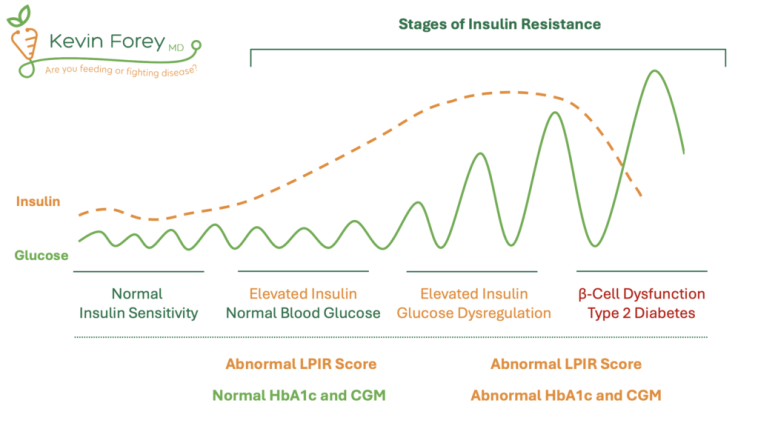
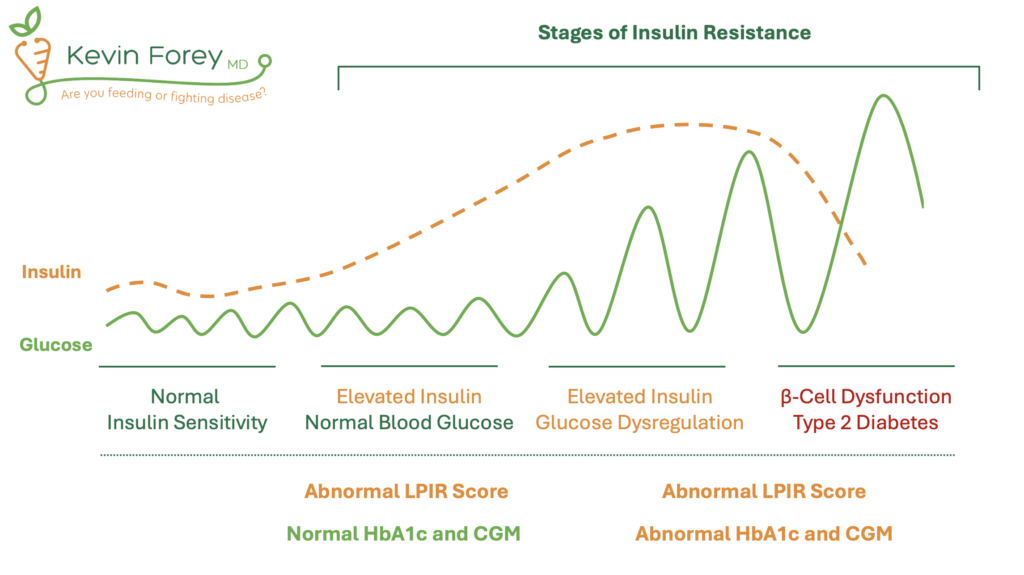
For years, HbA1c has been recognized as a key marker in diabetes management, helping clinicians figure a path through the maze of tracking glycemic status over time. However, when patients carry underlying conditions that affect red blood cell dynamics—like thalassemia trait—the method can produce unexpectedly low or misleading values. This case clearly shows that even when blood glucose levels and clinical symptoms paint a picture of significant hyperglycemia, HbA1c might be way off the mark.
Understanding the Blood Test Gap
Hemoglobin A1c reflects the average blood glucose over roughly two to three months, a window that helps patients and healthcare providers manage long-term glycemic control. But here’s the catch: any condition that affects red blood cell turnover can interfere with HbA1c readings. Thalassemia trait, which alters both the lifespan and structure of red blood cells, is one of these conditions. As a result, the small details in the lab values might not match up with the patient’s clinical presentation.
In the case we are discussing, despite evident hyperglycemic symptoms and evidence of diabetic ketosis (high blood sugar combined with ketones), the patient’s HbA1c was surprisingly low—around 2.3%, well beyond the expected range for someone with uncontrolled diabetes. Such a blatant discrepancy forces us to re-examine our reliance on HbA1c when faced with certain hematologic conditions.
Identifying the Hidden Complexities of Hemoglobinopathies
The presence of thalassemia trait presents a nerve-racking scenario for both clinicians and laboratory specialists. It is a vivid reminder that even widely accepted diagnostic tests have their subtle pitfalls. While HbA1c has proven to be reliable in most scenarios, its limitations become painfully clear when patients present with hemoglobin variants or altered red blood cell life cycles. In these cases, lab results can be loaded with issues that may lead providers to underestimate the severity of diabetes or delay crucial treatment interventions.
Thalassemia Trait and the Mystery of Misleading Results
When a patient with thalassemia trait undergoes an HbA1c test, the abnormal red blood cell turnover can cause the measurement to read deceptively low levels. This misleading reading occurs because the test relies on the glycation of hemoglobin that accumulates over the lifespan of red blood cells. When this lifespan is cut short by conditions like beta-thalassemia, the amount of glycated hemoglobin is reduced—even if the blood sugar is consistently high.
This situation creates a dangerous twist: clinicians might be fooled into thinking that glycemic control is better than it actually is, leading to a potential under-treatment of diabetes. In regions with a high prevalence of thalassemia, such as Kuwait, this misinterpretation can have significant public health implications.
Alternative Strategies for Reliable Glycemic Monitoring
Given the inherent twists and turns in using HbA1c for patients with thalassemia trait, it is critical to explore alternative monitoring strategies. Relying only on one biochemical marker may lead to misdiagnosis or delayed treatment. Fortunately, several alternative methods can offer clarity when the standard tests fall short.
Continuous Glucose Monitoring: A Dynamic Approach
Continuous glucose monitoring (CGM) has emerged as an essential tool in cases where the HbA1c test is less reliable. Unlike HbA1c, which provides a retrospective average of blood sugar levels, CGM offers real-time data. With sensors placed just under the skin, CGM gives a detailed picture of blood glucose trends over time—capturing the fine shades and subtle details of glycemic variations with impressive accuracy.
This approach is particularly useful in patients with hemoglobinopathies since CGM readings remain unaffected by red blood cell turnover or hemoglobin variants. Healthcare providers can rely on this method to make timely and informed decisions regarding insulin dosing and other therapeutic adjustments. Some key benefits of CGM include:
- Real-time tracking of glucose fluctuations
- Diminished need for frequent finger-stick tests
- Ability to set alerts for hypo- and hyperglycemia
- Detailed reports that help in fine-tuning treatment plans
Serum Fructosamine: A Short-Term Indicator
Another interesting alternative is the measurement of serum fructosamine. Unlike HbA1c, fructosamine levels reflect glycemic control over a shorter period—usually two to three weeks. This marker measures the glycation of serum proteins, predominantly albumin. It can be particularly valuable for patients who are undergoing frequent adjustments in their diabetes management plan or who have conditions that might skew longer-term glycemic assessments.
While fructosamine is not as commonly used as HbA1c, it remains a practical choice in scenarios where hemoglobin-based assessments are compromised. It’s essential, however, to keep in mind that factors such as liver disease or low albumin levels might affect fructosamine results, meaning this method, too, is not without its own complications.
Unlocking the Lab Results: Practical Tools and Techniques
Interpreting lab results in patients with microcytic anemia isn’t always straightforward. In scenarios like this, several practical tools can help untangle the confusing bits of diagnostics. One such valuable metric is the Mentzer index, which helps distinguish between thalassemia trait and iron deficiency anemia.
Using the Mentzer Index for Accurate Diagnosis
The Mentzer index is calculated by dividing the mean corpuscular volume (MCV) by the red blood cell (RBC) count. In our patient’s case, the index was significantly below 13—a value that supports the diagnosis of thalassemia trait. This index is a simple, cost-effective tool, especially useful in regions where thalassemia is common.
Here’s an example table outlining the laboratory results from the case:
| Parameter | Obtained Value | Reference Range |
|---|---|---|
| Fasting Blood Glucose | 25 mmol/L | 3.9–5.5 mmol/L |
| Serum Ketones | 3.0 mmol/L | <0.6 mmol/L |
| pH (Venous Blood Gas) | 7.40 | 7.35–7.45 |
| Bicarbonate | 20 mmol/L | 22–28 mmol/L |
| Red Blood Cells | 6.86 | 4.5–5.5 (million cells/µL) |
| Hemoglobin | 121 g/L | 135–175 g/L |
| Hematocrit | 0.372 | 0.4–0.5 |
| Mean Corpuscular Volume (MCV) | 54 fL | 80–96 fL |
| Reticulocyte Count | 2.9% | 0.5–2.5% |
| Total Bilirubin | 12 µmol/L | 5–21 µmol/L |
| HbA1c (Initial) | <2% | 4.0–6.0% (non-diabetic) |
| HbA1c (Repeat) | 2.3% | 4.0–6.0% (non-diabetic) |
The high RBC count, low MCV, and a Mentzer index calculated as 7.87 all pointed toward thalassemia trait rather than iron deficiency, further clarifying the difficulty of interpreting HbA1c results in this context. Recognizing these small distinctions is crucial in tailoring diabetes management strategies effectively.
Tailoring Diabetes Management in Complex Cases
Once the discrepancy between glycemic markers is recognized, healthcare providers need to retool their approach, steering through this maze of conflicting results with a method that involves more personal, patient-centric care. In the case under discussion, relying on CGM provided real-time data that allowed for precise adjustments in insulin therapy. Over the course of eight weeks, with consistent basal-bolus insulin management guided by continuous readings, the patient’s glycemic control improved notably.
Considerations When Adjusting Treatment Plans
When faced with discordant lab results, several steps can be followed to ensure proper diabetes management:
- Review Clinical Presentation: Always correlate laboratory findings with the patient’s symptoms. If a patient exhibits evident hyperglycemic symptoms with ketonuria, a normal or low HbA1c should raise red flags.
- Use Alternative Markers: Employ continuous glucose monitoring or serum fructosamine tests to get an accurate, real-time view of glycemic control.
- Consider Hemoglobinopathies: Factors like thalassemia trait should be suspected in regions with a high prevalence of these genetic traits. In such cases, screening tools like the Mentzer index become incredibly useful.
- Adjust Therapy Dynamically: Base adjustments in insulin and other diabetes medications on multiple data points rather than relying solely on HbA1c.
This multi-pronged approach ensures that the treatment plan is both holistic and personalized—a critical necessity when clinical findings are as complicated as they were in this case.
Diving into the Role of Laboratory Techniques and Correction Formulas
Another angle that deserves attention is the use of correction formulas and the influence of various lab techniques on HbA1c readings. Some researchers have proposed equations to estimate a corrected HbA1c in the setting of significant anemia. For example, one formula is:
Corrected HbA1c = Measured HbA1c + (15 – Hemoglobin in g/dL) × 0.4
While such correction methods may offer some guidance, they are not yet validated for routine clinical practice. In patients where anemia is more severe, these formulas might provide an added layer of insight, but in cases of mild anemia (as seen with our patient who had a hemoglobin level around 121 g/L), the correction might not be necessary. The key takeaway is that these mathematical adjustments can sometimes help figure a path through the maze, but they should be used alongside solid clinical judgment and additional real-time monitoring tools.
Examining the Small Details: Lab Assay Influence
Molecular techniques like ion-exchange high performance liquid chromatography (HPLC) are commonly used to measure HbA1c. However, these methods can be susceptible to interference from abnormal hemoglobin variants. In patients with thalassemia trait, where the quality and turnover of red blood cells are altered, the HPLC assay might inadvertently produce figures that do not reflect the true glycemic status.
This phenomenon serves as a reminder that even sophisticated lab techniques can have hidden complexities. Clinicians must be careful and consider cross-checking results using alternative methods such as capillary blood glucose assessments or CGM data to get a full picture. In regions with a high prevalence of hemoglobinopathies, combining multiple methods is often the most practical strategy for obtaining reliable data.
Regional Considerations and Public Health Implications
In areas such as Kuwait, where thalassemia traits are not uncommon, the diagnostic pitfalls associated with HbA1c misinterpretation are especially important. Local prevalence rates of beta-thalassemia trait are estimated to be over 2%, with alpha-thalassemia affecting up to 40% of the population. These striking statistics underscore the need for healthcare providers in such regions to be extra attentive when interpreting common diabetes tests.
Approaches for Medical Practitioners in High-Risk Regions
For practitioners managing diabetes in regions with elevated thalassemia rates, the following strategies can be particularly helpful:
- Routine Hemoglobinopathy Screening: Consider including tests for hemoglobin variants in the workup of patients suspected of having diabetes, especially if clinical signs and HbA1c readings do not correlate.
- Educate and Train Staff: Ongoing training and awareness programs about the tricky parts of diabetes diagnosis in the context of hemoglobin disorders can empower clinical teams to catch potential discrepancies early.
- Invest in Alternative Monitoring Tools: Allocating resources toward continuous glucose monitoring systems and ensuring their availability at diabetes clinics can help in capturing the real-time data that is often missing when relying solely on HbA1c.
- Collaborate Across Departments: Endocrinologists, hematologists, and laboratory professionals should work closely to manage patients with overlapping conditions, ensuring that every piece of the diagnostic puzzle is taken into account.
Adopting these strategies not only serves individual patient needs but also has significant public health benefits by preventing misdiagnoses and supporting proactive, patient-centered diabetes management initiatives across the community.
Patient-Centered Perspectives: The Human Side of Laboratory Testing
Beyond the technical details and laboratory algorithms, patient care remains at the core of all these debates. The moment when a patient learns that their HbA1c does not reflect their actual blood sugar status can be incredibly overwhelming. For many, the news that their test results are unreliable may be both intimidating and confusing. It is during these times that a compassionate, nuanced explanation from healthcare providers can make all the difference.
Empowering Patients Through Education
It is super important to help patients understand that no diagnostic test is perfect on its own. Rather, tests function as tools—each with its own set of advantages and limitations. When a familiar test like the HbA1c produces unexpectedly low results in the face of clear clinical symptoms, patients should be informed of the reasons behind such discrepancies. Explaining that their condition might affect the reliability of conventional assays helps reduce the fear and uncertainty that often accompanies unexpected laboratory findings.
By actively involving patients in discussions about alternative monitoring approaches—such as continuous glucose monitoring or serum fructosamine testing—clinicians can empower patients to take an active role in their diabetes management. This collaborative approach improves adherence to treatment plans and encourages patients to engage with their own care because they know the reasoning behind each decision.
Taking the Wheel: Making Informed Therapeutic Decisions
In practice, the case we are reviewing required a significant change in management once it became clear that HbA1c values were unreliable. With a strong reliance on CGM, the treatment plan was quickly revised. Insulin therapy was adjusted based on accurate, real-time blood sugar readings rather than on potentially misleading long-term averages. This thoughtful response highlights a broader point: in medicine, one must often take a closer look at standard protocols and be ready to switch gears when the clinical situation calls for it.
Key Steps for Clinicians to Consider
When faced with unexpected or discordant test results in diabetes management, here are some practical steps to figure a path through the maze:
- Reassess the Entire Clinical Picture: Look at symptoms, laboratory data, and patient history together rather than in isolation.
- Confirm with Repeat Testing: When one test raises questions, re-testing can help verify whether an anomaly is persistent or simply a one-off laboratory error.
- Employ a Combination of Monitoring Tools: Do not rely solely on HbA1c; incorporate CGM data, self-monitoring blood glucose logs, or serum fructosamine measurements to gain a clearer overall picture.
- Consult With Specialists: Collaboration with hematologists can clarify whether underlying hemoglobinopathies might influence glycemic markers.
Following these steps can help ensure that the therapeutic approach is well-rounded, safe, and tailored to the individual needs of the patient.
Looking Ahead: The Future of Diabetes Testing
The issues raised by this case are not just isolated problems—they symbolize a larger challenge in modern medicine: the need to continuously update our methods as new evidence emerges. Relying solely on HbA1c for long-term glycemic assessment may be too simplistic, especially in a world where genetic and ethnic diversity bring about varied clinical presentations. The need to integrate multiple modalities for accurate diagnosis and management is clearer now than ever before.
Innovations on the Horizon
As technology evolves, we can expect improvements in both the design and reliability of glycemic markers that are independent of hemoglobin quality or red blood cell turnover. Future research may yield novel biomarkers and diagnostic tools that bypass the current limitations seen with HbA1c. For example:
- Advanced Biosensors: New devices might combine multiple parameters into a single, refined index that is less affected by underlying hemoglobin disorders.
- Genetic Marker Integration: Incorporating a patient’s genetic profile could allow for personalized correction algorithms, improving accuracy.
- Innovative Imaging Techniques: Although still experimental, imaging methods that assess tissue glycation might one day complement traditional blood tests.
Such developments will not only improve diagnostic accuracy but also empower healthcare providers to offer truly individualized care, ensuring that no patient is left behind because of atypical laboratory responses.
Conclusion: Embracing a Multi-Faceted Approach for Better Diabetes Care
The case of unexpectedly low HbA1c in a patient with new-onset diabetes and beta-thalassemia trait is a stark reminder that even the most trusted tests have their limits. When a test that has long been considered the gold standard gives results that do not match the clinical scenario, it is a sign that medical professionals need to step back and reconsider the diagnostic strategy.
Through our discussion, we have seen how conditions that affect red blood cell turnover—like thalassemia trait—can lead to confusing bits in laboratory data. It is clear that alternative approaches such as continuous glucose monitoring and serum fructosamine measurements provide a better real-time snapshot of glycemic control in these instances. Moreover, simple tools like the Mentzer index can help untangle the complicated pieces of the diagnostic puzzle by distinguishing between thalassemia and iron deficiency anemia.
This case urges us to avoid a one-size-fits-all approach in medicine. Instead, clinicians should steer through the maze of diagnostic data with flexibility, creativity, and continual learning. By embracing a multi-faceted diagnostic strategy, we can make well-informed decisions that improve patient outcomes and personalization of care. The responsibility falls on all healthcare providers to recognize when standard tests might be misleading and to be proactive in seeking ways to ensure that the treatment plan truly aligns with the patient’s clinical reality.
Ultimately, as we work through these tangled issues, continuous education, innovative diagnostic techniques, and improved collaboration between specialties are essential. In the rapidly evolving landscape of diabetes care, staying updated on both the capabilities and the limitations of our diagnostic tools is not just a professional obligation—it’s a critical component of compassionate, accurate, and effective patient care. As we continue to dig into the fine points of diabetes management in patients with hemoglobinopathies, let us champion a system that values precision, adaptability, and the human side of healthcare, ensuring that every patient receives a diagnosis and treatment plan that truly addresses their unique needs.
In summary, while HbA1c remains a cornerstone for evaluating long-term glycemic control, its limitations in the setting of hemoglobinopathies call for alternative monitoring techniques. As practitioners, we must be ready to adjust our methods, rely on a comprehensive clinical correlation, and use the best available tools—whether that means tapping into the real-time insights from CGM or employing serum fructosamine measurements. This patient-centered approach not only safeguards against misdiagnosis but ultimately provides a more secure foundation upon which to build effective, personalized diabetes care.
Let this case be a reminder that in medicine, like in life, it is crucial to recognize when our trusted measures might fail us— and to be nimble enough to find another way. Only by being aware of the twists and turns, the subtle details, and even the unexpected low points in our lab results can we ensure that our approach to diabetes management remains as dynamic and responsive as the patients we serve.
Originally Post From https://www.cureus.com/articles/378687-unexpectedly-low-hba1c-in-a-patient-with-newly-diagnosed-diabetes-mellitus-and-thalassemia-trait-a-case-report
Read more about this topic at
Diagnostic Dilemma of HbA1c Detection in Presence of a …
Diagnostic Dilemma of HbA1c Detection in Presence of a …