Personal Experience with Prostate Cancer Screening and The Silent Epidemic
My encounter with prostate cancer screening was a wake-up call—a reminder that hidden health issues might not show obvious signs until they’ve advanced. I remember the day clearly: my doctor’s familiar instruction to lower my boxers, bend forward, and brace my elbows on the table. A digital rectal exam (DRE) was underway, a procedure both nerve-racking and, in its own way, revealing. Although the exam itself was over in no more than a handful of seconds, it set off a chain of events that forced me to take stock of my health and the subtle details of prostate cancer screening.
In the United States, prostate cancer is often dubbed “the silent epidemic.” While many view it as one of the lesser evils among cancers, its hidden complexities and the potential for severe consequences cannot be understated. As a 67-year-old technology executive, jazz pianist, and memoir writer, I now appreciate that early detection is a must-have tool to save lives. Reflecting on my own journey, I have come to realize that even an active lifestyle, a plant-based diet, and regular health check-ups may not be enough without the right medical screenings.
The Importance of Annual Physicals and PSA Discussions
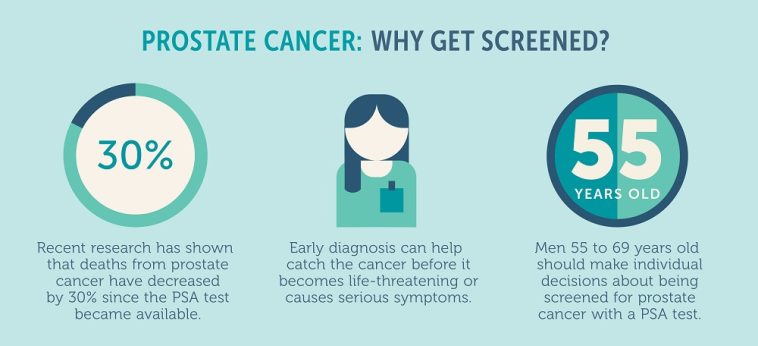
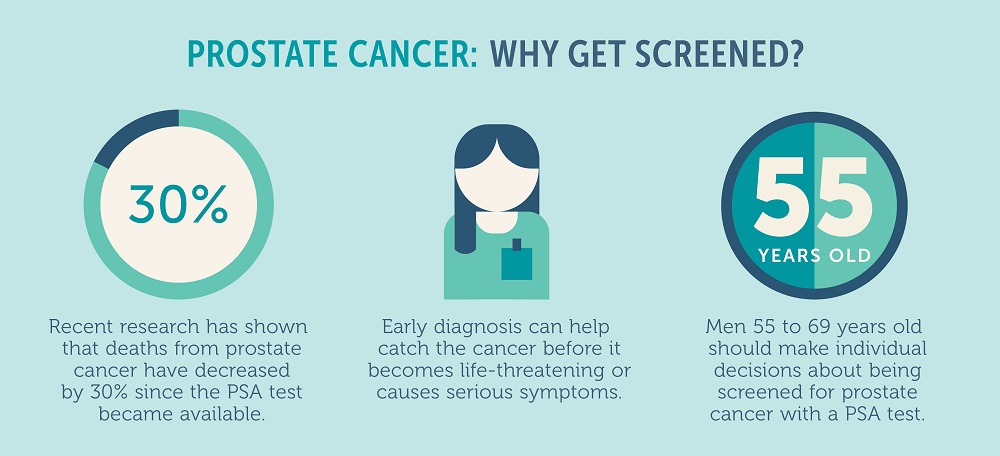
Annual physical check-ups are more than just routine appointments—they are crucial opportunities to discuss potential health risks that change as we age. For men, especially those over 50, conversations about prostate health and the role of PSA (prostate-specific antigen) tests are super important. I regret that I once dismissed my health as bulletproof until circumstances forced me to pick up a new primary care physician.
Before my 62nd birthday, it was easy to push aside the annual physical. I had always been athletic, shunning cigarette smoke and processed foods, convinced that my well-ordered lifestyle shielded me from serious diseases. However, once I returned to regular check-ups, it became clear that even for those in good shape, the tricky parts of aging—especially those involving silent diseases like prostate cancer—could play a devastating role.
A routine PSA test, which measures a protein produced by both healthy and potentially cancerous prostate cells, can provide early hints of trouble. Although elevated PSA levels do not automatically spell cancer, they signal that further investigation may be necessary. This test has its own set of hidden complexities. For instance, PSA values vary from person to person, and factors such as family history and overall health can affect how these values are interpreted year by year.
Understanding Prostate Health: The DRE Experience
The digital rectal exam (DRE) is one of those procedures that many describe in terms ranging from simply uncomfortable to downright nerve-racking. Its purpose is straightforward—to physically check the prostate for lumps, nodules, or regions that feel unusually hard. Though the examination itself is quick, the anxiety it generates can linger longer than the process itself.
This exam is a tangible reminder of how vulnerable our bodies can be to hidden issues. The gland’s location, nestled just below the bladder and in front of the rectum, makes it difficult to assess thoroughly without such exams. For many men, the DRE remains one of the few moments when the reality of potential health issues becomes unmistakably clear.
While I was relieved when my doctor reassured me that everything felt normal at first glance, I was still unaware of the tangled issues that arise with prostate cancer, especially with advancing age. The DRE, like many health procedures, has subtle parts that require both medical expertise and patient understanding. It is not just about detecting lumps—it is about recognizing the many small twists and turns that accompany the aging process.
Examining PSA Testing: Hidden Complexities and False Alarms
Once I transitioned to a new physician, my introduction to the PSA test marked the next significant turning point in my health journey. The PSA test, though common, brings with it a host of fine points that can add to patient anxiety. As with any diagnostic tool, there are benefits and risks. The protein produced by the prostate helps differentiate between normal and potentially cancerous activity, but it is not a foolproof test.
Here are some of the twisted issues associated with PSA testing:
- False Positives: Elevated PSA levels might indicate issues that are not cancer, such as infections or inflammation. This can lead to further testing like biopsies, which might prove nerve-racking and cause undue stress.
- False Negatives: There are instances when the test shows normal levels even in the presence of prostate cancer. According to experts, a surprising percentage of men with normal PSA levels might still have undetected cancer.
- Overdiagnosis: Some slow-growing cancers may never cause significant harm during a man’s lifetime. However, detecting these “benign” cases can lead to treatments that expose patients to complications like urinary leakage, erectile dysfunction, and other quality-of-life issues.
Understanding these confusing bits of information can be overwhelming. Yet, they are crucial for making informed decisions. Physicians often emphasize that while a PSA test is a handy tool, its results should be interpreted on a case-by-case basis. Changes in a patient’s dosage over time, rather than one isolated reading, can be key to understanding whether further tests or treatments are necessary.
Experts like Dr. Ash Tewari, who leads the urology department at Mount Sinai, stress that tracking PSA levels annually can help identify small distinctions that might otherwise go unnoticed. This careful monitoring can provide essential clues about whether the changes are part of a benign process or an early sign of cancer.
Risks vs Benefits: Weighing Treatment Options and Their Consequences
When faced with a cancer diagnosis, every decision can feel laden with confusing bits and numerous implications. I found myself grappling with emotions and facts that were all too familiar—the dread of potential treatments and the possibility of unwanted side effects. In my case, a radical robotic nerve-sparing prostatectomy was the final step following a confirmed diagnosis.
The treatment options available today range from surgery and radiation to newer, minimally invasive techniques. However, every choice comes with its own set of pros and cons:
- Surgery: Procedures such as the nerve-sparing prostatectomy are designed to remove the cancer while preserving urinary and sexual function. Still, they come with risks of long-term incontinence and erectile dysfunction.
- Radiation Therapy: This is another common treatment. While it can target cancer cells, radiation can also lead to issues like loose stools, rectal bleeding, and other complications.
- Minimally Invasive Techniques: Emerging methods such as high-intensity focused ultrasound (HIFU) are becoming more popular because they are less invasive and aim to preserve normal bodily functions as much as possible.
Making your way through treatment decisions is loaded with issues. Many men must weigh the immediate benefits of early detection against the potential long-term risks associated with treatment. While early screenings like the PSA test have been credited with saving lives, the possibility of overdiagnosis and the resultant psychological and physical stress remain significant concerns.
The treatment side effects, like impaired sexual function or continence issues, can have ripple effects on everyday life. Men often describe the period after treatment as a time full of problems—both physical and emotional. Thus, it is essential for patients to have detailed discussions with their healthcare providers to work through these decisions, balancing potential benefits against the nerve-racking risks.
Expert Opinions: Listening to Medical Professionals Amid Confusing Bits
Across the country, leading urologists and oncologists are weighing in on the debate about prostate cancer screening. There is no single answer to the question of when to test and when to treat. Many experts advocate for a balanced approach—encouraging men to consider their individual risk factors before making decisions.
For example, Dr. Samuel L. Washington, an esteemed urologic surgeon at the University of California in San Francisco, warns that prostate cancer can develop silently even in those who lead active lives. “Many men with prostate cancer won’t experience any outward signs or symptoms until the disease is advanced,” he notes, emphasizing that the subtle details of early detection are too important to ignore.
On the other hand, opinions differ when it comes to the PSA test itself. Dr. Nancy L. Keating, a professor at Harvard Medical School, points out that while screenings can offer a modest benefit, the potential side effects from unnecessary biopsies or treatments might outweigh the gains. In one study involving over 400,000 men, the small reduction in mortality was counterbalanced by the anxiety and physical complications that arose among many men.
These expert insights are a reminder that every decision, no matter how should be made on a case-by-case basis. Some men—particularly African American men or those with a family history of prostate cancer—may benefit more from early and regular screening. For others, a targeted strategy based on individual risk may be the best route. Both views carry weight, and the key lies in discussing subtle details with a trusted healthcare provider.
Below is a table summarizing some of the key factors considered in evaluating prostate cancer screening:
| Factor | Considerations |
|---|---|
| Age | Men over 50 generally face greater risk, but younger men with genetic predispositions also need careful attention. |
| Family History | A strong family history of prostate cancer may signal an increased need for regular screening. |
| PSA Level Trends | Year-to-year changes are more critical than a one-time measurement. |
| Race and Genetics | African American men and those with genetic mutations such as BRCA1/2 have heightened risk. |
| General Health | Existing conditions and overall lifestyle factors can influence diagnosis and treatment options. |
Emerging Techniques in Prostate Cancer Treatment and Their Benefits
The landscape for prostate cancer treatment is evolving, and emerging techniques offer new hope for those diagnosed. Modern methods such as high-intensity focused ultrasound (HIFU) provide minimally invasive alternatives to traditional surgery. By using targeted sound waves to destroy cancer cells, HIFU minimizes damage to surrounding tissues, reducing the risk of issues like incontinence and erectile dysfunction.
These techniques not only provide a better quality of life post-treatment but also offer significant benefits when used as part of early detection strategies. Urologists have noted that when the timing is right, these options help steer through the tricky parts of treatment without compromising efficacy. They allow for a more focused approach, dealing with the fine points and little details of each patient’s condition.
Additionally, the adoption of improved imaging techniques, such as MRI-guided biopsies, has revolutionized the way doctors figure a path through prostate cancer detection. For example, instead of relying solely on the PSA test, doctors can now obtain detailed imaging that pinpoints the existence and location of tumors with much greater accuracy. This combination of screening methods ensures that treatment can be as targeted and precise as possible, significantly lowering the chance of undertreatment or overtreatment.
With these innovations, the decision-making process regarding screening and treatment becomes a bit more straightforward. The fact that there are choices available, tailored to individual circumstances, gives patients a sense of control—an absolute necessity when dealing with an issue that affects so many lives.
Tips for Men: How to Make Informed Decisions About Your Health
For any man navigating the maze of prostate cancer screening and treatment, gathering complete and reliable information is super important. While the medical community remains divided on some screening methods, there are several key steps that can help you figure a path through this full-of-problems landscape.
Here are some practical tips:
- Talk to Your Doctor: Whether it’s about the PSA test or the DRE, have an open conversation about what to expect, the potential benefits, and possible side effects. Asking the right questions can help clear up those confusing bits.
- Know Your Family History: If prostate cancer runs in your family, it might be wise to begin regular screenings earlier. Being proactive can make the difference between catching cancer early and letting it progress unnoticed.
- Monitor PSA Trends: Rather than fixating on one test result, focus on how your PSA levels change over time. Regular tracking provides key insights into subtle shifts that might be cause for further investigation.
- Consider Additional Tests: Advanced imaging techniques, like MRIs, offer a complementary view to blood tests. These tools help pinpoint any suspicious areas with much finer detail.
- Evaluate All Treatment Options: Understand the potential outcomes and side effects of each treatment. Whether it’s surgery, radiation, or newer techniques like HIFU, each option has its own set of pros and cons that should be matched to your individual lifestyle.
Educating yourself about these little twists is off-putting but necessary. The more you know, the better you can work through the tangled issues and find the health solutions that best work for you.
Balancing Screening Benefits Against the Risks of Overdiagnosis
One of the most nerve-racking aspects of prostate cancer screening is the risk of overdiagnosis. Many men undergo the PSA test only to discover that they have a slow-growing cancer that might never have caused any real harm. While this early detection might sound like an unmitigated benefit, the resulting treatments can sometimes lead to significant, long-term side effects.
Overdiagnosis may lead to treatments that produce complications such as:
- Urinary incontinence, which can affect daily life in unexpected ways.
- Erectile dysfunction, a side effect that carries substantial emotional and psychological weight.
- Exhaustive treatments that may have been unnecessary in hindsight.
It is essential to sort out these details with your healthcare provider. A critical conversation about how to interpret PSA results and whether to proceed with further testing is necessary for managing your health wisely. Both studies and expert opinions suggest that the small benefit of saving a few lives must be weighed against these unwanted side effects. In some cases, the test may even lead to regret later on—something that many men have reported after undergoing a prostate biopsy that turned out unnecessary.
Managing Your Way Through Confusing Bits: A Patient-Centric Approach
When faced with a potential prostate cancer diagnosis, you’re not alone in feeling overwhelmed. The process—from the initial screening to navigating through various treatment decisions—is loaded with issues that can seem both intimidating and overwhelming. The key is to take a closer look at all the available options and work closely with your doctor to manage your way through these periods of uncertainty.
Here are some steps to help ease the journey:
- Stay Informed: Access reliable and up-to-date information about prostate cancer and screening methods. Medical journals, reputable health websites, and second opinions from specialists can all contribute to a well-rounded understanding.
- Communicate Openly: Don’t hesitate to ask your provider to explain the fine points of your test results. Make sure you understand the small distinctions between various PSA levels and what they might mean.
- Assess Emotional Impact: Consider speaking with a counselor or joining a support group for men who have faced similar issues. The emotional toll of a cancer diagnosis is real, and sharing experiences might offer relief from anxiety.
- Create a Health Plan: Work with your doctor to outline a personalized health strategy that considers your family history, lifestyle, and overall well-being. Establishing clear next steps can help steer through the nerve-racking timeline of diagnosis and treatment.
By prioritizing your health with a patient-centered approach, you not only gain a clearer view of the subtle details involved in screening but also place yourself in a stronger position to make informed decisions that affect your long-term well-being.
Reflections on a Life-Saving Test: The Role of Early Detection
The narrative of my own prostate cancer journey is a testament to the fact that early detection saves lives. Although my first exposure to the PSA test injected me with a degree of anxiety, it ultimately provided a second chance—a reminder that no type of cancer should ever be considered “the best to have.” Instead, every cancer carries risks, and early screening is a key part of mitigating those risks.
Looking back, the timing of my diagnosis was both a blessing and a burden. I recall feeling the dread of the biopsy procedure, much like the intense fear one might associate with getting a root canal after years of neglecting dental care. Yet, the brief discomfort was a small price to pay for the opportunity to tackle a dangerous disease head-on. Had I waited any longer, the cancer might have spread beyond the prostate membrane, limiting the treatment options available.
The truth is that early detection through routine screening can make all the difference when it comes to managing prostate cancer. It opens the door for a variety of treatment options, some of which are far less invasive than others. For patients like me, recognizing the small shifts in health metrics at an early stage can spell the difference between a manageable condition and a far more complicated, nerve-racking situation down the line.
The conversation around prostate cancer screening is ongoing, and while there is no one-size-fits-all solution, it is clear that staying proactive about one’s health is essential. Through regular consultations, consistent monitoring, and emerging innovations in treatment, we can work to find our way through the confusing bits of prostate health.
Looking Ahead: The Future of Prostate Cancer Screening and Treatment
As research continues to refine the methods used to detect and treat prostate cancer, the future holds promise for better outcomes and more personalized care. The development of advanced imaging techniques, minimally invasive therapies, and more precise tests will likely reduce the current challenges associated with overdiagnosis and false positives.
Looking ahead, here are several emerging trends to watch:
- Improved Diagnostic Accuracy: New biomarkers and advanced imaging are poised to help figure a path through the twists and turns of diagnosis. These advancements aim to reduce the rate of both false positives and negatives, offering patients a clearer picture of their health status.
- Personalized Treatment Plans: With genetics and family history playing a more central role in treatment decisions, personalized medicine continues to grow in importance. Tailoring treatment plans to the individual will help minimize unwanted complications.
- Minimally Invasive Options: Techniques like HIFU and robotic-assisted surgeries are becoming more refined, promising reduced side effects and a quicker return to normal life after treatment.
- Holistic Approaches: Increasingly, healthcare providers recognize the importance of integrating physical, emotional, and nutritional guidance in patient care, ensuring that treatment is not just about addressing the cancer, but about improving overall quality of life.
These advances underscore how essential it is to have an open dialogue with your healthcare provider. Regular screening may seem intimidating at first, but the emerging trends in both technology and treatment aim to make the process less overwhelming. As these trends develop, they will likely offer more effective ways to monitor and manage prostate cancer, ensuring that more men can avoid the nerve-racking outcomes of an advanced disease.
Conclusion: Embracing Informed Choices and a Proactive Approach
In conclusion, the journey through prostate cancer screening and its subsequent treatment is paved with both promise and challenges. It is clear that while screening tests like the PSA are not without their drawbacks, their role in early detection is super important. My personal experience—and the shared insights from medical experts—demonstrate that early intervention can indeed be life-saving.
The key takeaway is to stay informed. Whether through regular annual physicals, detailed discussions regarding PSA test results, or exploring emerging treatment options, understanding the little details of prostate health can empower you to take control of your future. Although the process might be intimidating, and the choices can be confusing, making your way through the tangled issues with the support of knowledgeable healthcare providers remains a critical part of modern medicine.
If there’s one lesson that I’ve learned through this journey, it’s that early screening provides too many benefits to ignore. I now advocate for proactive health assessments, particularly for men over 50 or those with a family history of prostate cancer. The combination of routine PSA discussions, the DRE experience, and evolving treatment methods creates a roadmap that, while it may have its nerve-racking moments, can ultimately guide you to a healthier future.
In our age of advancing medical technology and increasingly personalized care, the confusing bits of prostate cancer detection are gradually being sorted out. With ongoing research and the debate among experts fueling new protocols, each patient stands to benefit from the improvements in both prevention and treatment.
Ultimately, the decision about whether to undergo screening should be made based on a balanced assessment of individual risk factors and informed discussions with your doctor. Whether you are just starting your early detection journey or are already navigating treatment options, remember that each step—no matter how small or nerve-racking—contributes to a greater understanding of your health.
By taking the time to dig into these issues and working through the tangled pieces of medical information, you can make educated choices that protect you today and in the years ahead. For me, the early detection of prostate cancer was a turning point, one that offered a second chance and a new lease on life. I encourage every man reading this to have those all-important conversations with their healthcare provider. It might just be the decision that saves your life.
Originally Post From https://www.theguardian.com/wellness/2025/aug/19/men-prostate-cancer-testing-pros-cons
Read more about this topic at
Cancer Screening Saves Lives | Crucial Catch | American …
Colorectal Cancer Screening Saves Lives