Opinion: No Outcome Without Access – Achieving Equitable Cancer Care Amid Rapid Advances
The landscape of oncology is transforming at a breathtaking pace. With precision oncology tools reshaping cancer diagnostics and treatment, there is a growing sense of optimism among clinicians and patients alike. However, the progress comes with its own set of tangled issues. Barriers such as inconsistent payer coverage, infrastructure setbacks, and social determinants of health (SDOH) combine to create a scenario where groundbreaking treatments risk remaining out of reach for countless patients. In this editorial, I aim to take a closer look at the challenges and opportunities in modern cancer care and how stakeholders might work together to ensure that innovation translates into real-world improvements.
The discussion centers around a key message voiced by many experts: “No outcome without access.” This rallying cry reminds us that even the best scientific breakthroughs can fall short if patients cannot easily access them. As a community that cares about everyone’s health, we must figure a path to ensure that advancements in technology and treatment are matched by practical support at every level—from genomic profiling to cellular therapies, and from community outreach to reimbursement strategies.
Embracing Precision Oncology Amid Tricky Parts of Implementation
The integration of genomic profiling, circulating tumor DNA (ctDNA), and minimal residual disease (MRD) testing are fundamentally changing how we treat a host of cancers. This fine-tuning of therapy selection improves treatment sequencing, response monitoring, and early detection of resistance. Yet, the real-world application of these tools still faces several complicated pieces that need addressing.
Real-World Impact of Genomic Profiling Tools
In specialties like breast, gastrointestinal, and gynecologic oncology, precision oncology tools are proving to be super important for guiding treatment. For instance, patients with rectal cancer and mismatch repair deficiencies are increasingly receiving neoadjuvant immunotherapy based on promising results from clinical trials such as the NICHE-2 study. The success of these treatments illustrates the potential of ctDNA and advanced genetic testing to shape treatment decisions in real time.
Yet, even as these tests become more routine, the challenges remain formidable:
- Inconsistent payer coverage, especially for repeat molecular testing, makes it nerve-racking for patients to access ongoing care.
- The integration of test results into electronic health records (EHRs) is not uniform, making it hard for clinicians to get around certain administrative delays.
- The internal costs of repeat genomic profiling could be reduced if integrated systems allowed seamless data sharing, yet many facilities still face off-putting infrastructure hurdles.
Olivia Aranha, MD, PhD, a respected oncologist, rightly pointed out that institutions need to invest in robust systems and collaborative frameworks. These enhancements not only standardize testing but also help in setting up a sustainable reimbursement strategy that choice patients from every background.
Barriers in Hematologic Cancers: Diagnosing and Treating Within Tight Time Frames
When we shift our focus to blood cancers, the stakes only get higher. The timely diagnosis and treatment of diseases like acute leukemia and multiple myeloma are critical for positive outcomes. In these conditions, decision delays can mean the difference between life and death.
Challenges in Malignant Hematology
In hematologic cancers, manufacturers and providers face several intimidating challenges:
- Diagnostic delays due to sendout testing at community sites can leave physicians with incomplete information when treatment decisions need to be made.
- Payer approvals for therapies such as chimeric antigen receptor (CAR) T-cell treatment can extend beyond two months. Such long waits are nerve-racking for patients with aggressive cancers.
- For clinical trial inclusion, patients from smaller communities or areas with limited resources often have to travel long distances to top-tier academic centers, creating additional logistical struggles.
Beyond treatment delays, the burden is compounded by paperwork that is frequently written at time-consuming reading levels. For many patients, consent forms and clinical trial directives are drafted in language that exaggerates the hidden complexities, leaving them overwhelmed and wary about participation. This calls for a critical review and subsequent revision of all patient-facing documents to ensure clarity.
Understanding Minimal Residual Disease Testing
Minimal residual disease (MRD) testing is gaining traction in determining the success of treatment in hematologic malignancies. By measuring the remaining disease burden post-treatment, MRD provides an actionable marker that could refine risk stratification. For a subset of patients with intermediate-risk disease, clearing mutations may mean they achieve outcomes similar to those with a favorable risk profile.
However, the use of MRD in tandem with newer treatments, such as bispecific antibodies, highlights another tricky part. While MRD-positive patients might benefit most, the challenges remain in synchronizing these diagnostics across various treatment lines. The fine balance between early application and cost-effectiveness continues to be a topic of debate among experts.
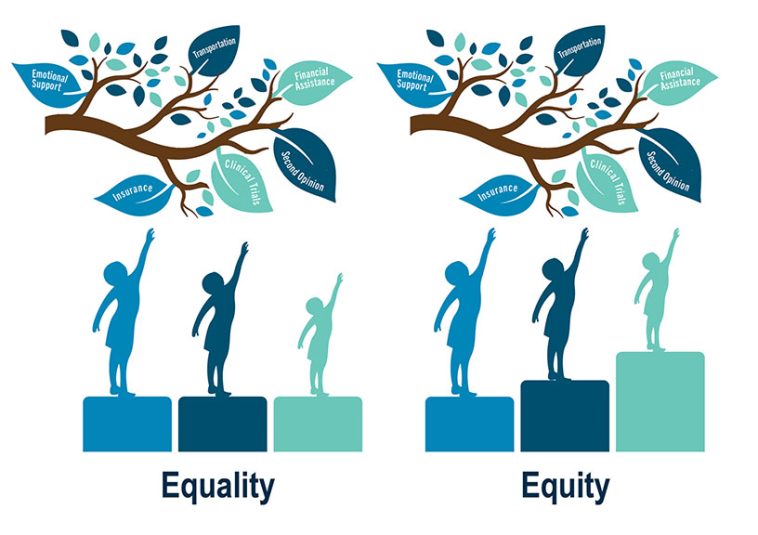
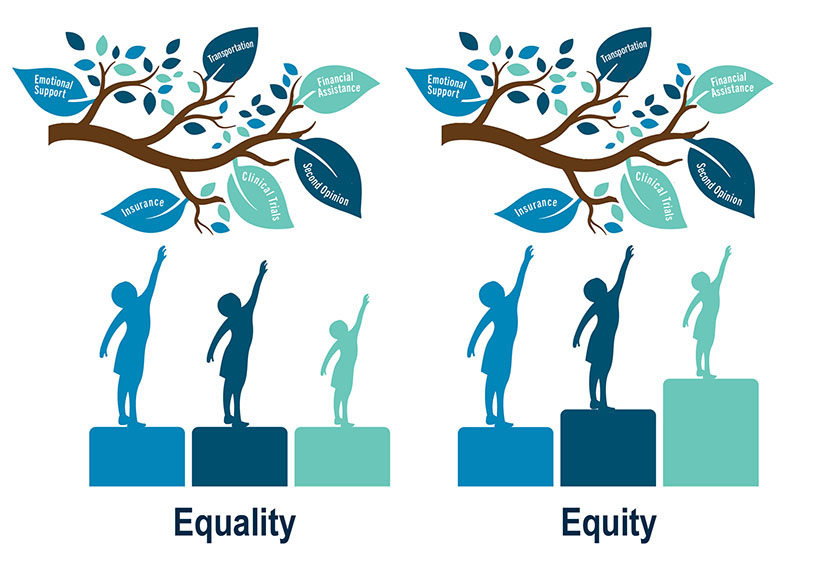
Social Determinants of Health: The Hidden but Critical Pieces
One of the central themes that emerged from recent discussions among oncology specialists is the significant impact of social determinants on the success of cancer treatment. When patients struggle to meet their basic needs, even the most advanced treatment plans can falter.
Addressing Food Insecurity and Transportation Barriers
Reports from clinics indicate that a startling number of patients suffer from food insecurity and transportation challenges. Anecdotes shared during professional meetings illustrate the reality: how can a patient focus on taking their medication if they are preoccupied with feeding their family?
This truth highlights three key factors that require immediate attention:
- Food Insecurity: Nearly one in three patients with breast cancer in some local studies reported a lack of access to nutritious food shortly after diagnosis.
- Transportation Challenges: Missed appointments due to lack of reliable transportation continue to impede treatment adherence.
- Financial and Job Instability: These add layers of stress and further complicate consistent treatment, particularly in rural and underserved communities.
Health systems and policymakers must find a way to work through these issues by integrating social work departments, offering transportation support, and ensuring that treatment environments address these life-threatening distractions. Initiatives such as providing local resource guides, transportation vouchers, and financial counseling can help steer through these challenges.
Securing Equitable Access to Cellular Therapies
CAR T-cell therapy represents one of the most exciting frontiers in cancer treatment. Despite its promise, the delivery and reimbursement landscape for these therapies is extremely loaded with issues that need immediate attention.
Overcoming Capacity Constraints in CAR T-Cell Delivery
According to recent estimates, although tens of thousands of patients could benefit from CAR T-cell therapy each year in the United States, fewer than 4,000 actually receive it. Many hurdles contribute to this gap:
- Distance and Eligibility: Patients often have to travel long distances to access specialized centers capable of delivering CAR T therapy.
- Caregiver Requirements: The intense aftercare, which may involve remaining outpatient for extended periods, risks excluding patients without strong local support systems.
- Reimbursement Challenges: Current Medicare guidelines, which penalize hospitals if a patient requires hospitalization post-infusion, force institutions to limit the number of CAR T infusions offered.
This scenario shows that while technological advancements are groundbreaking, the operational side is loaded with twists and turns. Hospitals often face potential financial losses ranging from $150,000 to $250,000 per patient in cases of inpatient care—a cost that many institutions simply cannot absorb. As a result, many hospitals turn to experimental or limited-scope programs, leaving community practices with insufficient resources to offer cutting-edge therapies.
Bispecific Antibodies: A More Scalable Alternative?
In contrast to CAR T-cell approaches, bispecific antibodies present an alternative that could be easier to scale. Although clinicians admit that there is some hesitancy during the initial ramp-up phase, the potential for quicker, more flexible administration may eventually reduce many of the nerve-racking challenges associated with CAR T-cell therapies.
Several key advantages make bispecific antibodies a promising complement to cellular therapies:
- Infrastructure Ease: They do not require the extensive specialized facilities needed for CAR T treatments.
- Cost Efficiency: With fewer logistical expenses and shorter administration times, bispecific antibodies might offer a more affordable alternative for community settings.
- Wider Accessibility: The simpler delivery methods could mean that more patients in rural or less resource-rich settings can gain access to these promising therapies.
Embracing bispecific antibodies might not just be a matter of clinical choice—it is also a strategic move aimed at narrowing the treatment gap and ensuring that innovations in cancer care are not confined to academic centers alone.
Enhancing Infrastructure to Support Advanced Oncology Diagnostics
The successful integration of precision medicine in oncology demands not only advanced technology but also a robust support system. A key aspect of overcoming the tricky parts of modern treatment is creating an IT infrastructure that can handle the influx of sophisticated diagnostic data.
Integrating Test Results into Electronic Health Records
One of the biggest bottlenecks today is the way test results are managed. Whether it’s genomic profiling or ctDNA assays, the outputs of these tests must be seamlessly woven into electronic health records (EHRs) to truly influence treatment decisions. Unfortunately, many systems are not yet up to the task—the fine points of interoperability remain a significant, often overwhelming challenge.
Here are several steps that institutions can consider:
| Action Step | Benefit | Potential Barrier |
|---|---|---|
| Invest in Custom EHR Modules | Ensures easy access to precision medicine data | High initial investment |
| Train Medical Staff on Data Integration | Improves usability and reduces errors | Time and resource intensive |
| Establish Data Sharing Protocols | Facilitates smoother transitions between treatment phases | Requires cross-departmental coordination |
By taking these steps, healthcare systems can transform the overwhelming and nerve-racking process of adapting new technology into a seamless part of daily care. As the data emerges quicker and more accurately within the clinical workflow, physicians can make well-informed decisions that favor the patient’s overall journey.
Working Through Insurance Barriers and Payer Policies
Even the most successful medical interventions can be rendered ineffective if insurance companies and payer policies are not aligned with modern practice. In oncology, ensuring that patients receive repeat molecular testing and other advanced diagnostics is super important but often hit by a wall of red tape.
Improving Reimbursement Models
Reimbursement challenges often add layers of intimidating, nerve-racking delays to patient care. For the promise of precision oncology to be fully realized, reimbursement models need to move from a one-size-fits-all approach to something more tailored and flexible.
Some suggestions to improve these models include:
- Sustainable Payment Structures: Payers should consider models that cover not only the initial treatment but also the essential repeat testing required to monitor and adjust care plans.
- Linking Reimbursement to Outcomes: By rewarding successful, evidence-based outcomes, insurers can help drive the adoption of innovative treatments while mitigating risk.
- Data-Driven Adjustments: Use ongoing data from EHRs and clinical trials to refine payer policies, ensuring that they reflect the latest scientific evidence and patient needs.
As stakeholders from every corner of the healthcare system work together, it is essential to recognize that these adjustments are not simply bureaucratic changes; they are vital for guaranteeing that medical breakthroughs have the desired real-world impact.
Community Outreach and Patient Education: Closing the Gap
Even as advanced therapies are developed, inequities in patient education and community outreach remain a pressing concern. Many patients find the transition from diagnosis to treatment filled with confusing bits, overwhelming paperwork, and subtle parts of the process that make it hard to get around the system.
Bridging the Health Literacy Divide
It has become increasingly evident that patients from diverse educational and socioeconomic backgrounds struggle with the nitty-gritty of understanding clinical trial consent forms, treatment plans, and advanced diagnostic reports. Healthcare providers must work on making these documents more accessible:
- Simplified Language: Create patient-facing materials that lower reading levels and focus on clear, concise language without compromising on accuracy.
- Visual Aids and Infographics: Graphical representations can help patients quickly grasp complex concepts.
- Community Workshops: Organize local sessions where experts can take a closer look at these issues and answer questions in an informal setting.
Social workers and patient navigators become super important in this environment, acting as liaisons who help patients sort out the many off-putting moments in their treatment journey. In doing so, they not only improve compliance but also reduce the sense of isolation that patients often feel when confronted with the subtle challenges of modern oncology.
Evaluating the Impact of Decentralized Clinical Trials
The traditional model of clinical trials is increasingly being questioned. In today’s world, many patients face intense challenges simply due to geographical limitations. Decentralized or hybrid trial models—where aspects of the trial take place remotely—offer a promising solution.
Decentralized Trials: Opportunities and Challenges
By leveraging technology to reduce the need for physical travel to academic centers, decentralized trials can make participation more accessible. However, these models also come with their own set of confusing bits that must be managed:
- Infrastructure and Technology: Reliable internet access and secure data platforms are essential, and these are not always uniformly available.
- Patient Engagement: Ensuring that patients understand remote trial procedures and maintain accurate reporting can be a delicate balance.
- Data Quality: There is a need to ensure that decentralized data is as robust as that collected in controlled, centralized environments.
With careful planning and the right technology investments, these challenges can be worked through. Industry leaders have stressed that decentralized trials may eventually become the norm, catalyzing a broader transformation in how we think about accessibility in clinical research.
Charting a Future of Collaborative Innovation in Oncology
At the heart of the transformation in cancer care is the belief that “innovation cannot achieve its potential without payer alignment, infrastructure investment, and concentrated focus on equity.” As healthcare providers, policymakers, and insurers work more closely together, there is immense potential to sculpt a system where every patient benefits from cutting-edge research.
The Role of Multi-Stakeholder Collaboration
Creating a seamless and accessible oncology care system calls for a unified effort. Here are some steps that can be taken to foster collaboration:
- Regular Multi-Disciplinary Meetings: Bring together clinicians, payers, IT specialists, and policy advisors to discuss practical solutions to current challenges.
- Public-Private Partnerships: Leverage the strengths of both governmental and industry efforts to build infrastructure, particularly in under-resourced areas.
- Educational Forums: Use platforms such as webinars and conferences to spread knowledge about best practices and innovative strategies.
By fostering such a collaborative spirit, stakeholders can streamline the process of integrating advanced diagnostics into everyday practice. This not only ensures that patients gain access to the best available treatments but also builds a resilient healthcare system that can adapt to future challenges.
Reaching a Consensus on Equitable Cancer Treatment
The discussion surrounding viable solutions is full of confident assertions and realistic expectations. Many experts emphasize that without a comprehensive approach—one that considers every angle of treatment, reimbursement, and social support—innovation in oncology will not translate into better outcomes for patients.
Key Takeaways for Moving Forward
Drawing on the myriad of insights shared at recent forums and clinical discussions, the following points are clear:
- Advanced diagnostics such as genomic profiling, ctDNA, and MRD testing are essential tools that must be integrated into patient care with reliable infrastructure support.
- Payer policies need to become more flexible and accommodating, ensuring that cutting-edge treatments are accessible to all patients, regardless of their socioeconomic backgrounds.
- Efforts to improve social determinants of health—through community outreach, patient education, and support programs—are as critical as any medical intervention.
- Decentralized clinical trials and scalable therapies like bispecific antibodies represent promising solutions that can help mitigate geographic and financial disparities.
- Collaboration between all stakeholders—clinicians, researchers, payers, and policymakers—is key to steering the future of equitable oncology care.
There is no silver bullet when addressing the tangled issues of modern cancer care. Instead, a multi-pronged strategy that tackles each challenge at its root is required. Only by acknowledging the real-world difficulties—be it off-putting documentation, nerve-racking reimbursement hurdles, or overwhelming transportation issues—can we hope to build a system that works for everyone.
Conclusion: A Call to Action for Equitable Cancer Care
The promise of precision oncology and advanced treatment modalities is a testament to human ingenuity and scientific progress. However, without a concerted effort to overcome insurance, infrastructure, and social barriers, these advances may risk remaining limited to well-resourced academic hubs.
By emphasizing collaboration and focusing on practical, real-world solutions, we as a healthcare community can figure a path forward. We are at a crossroads where the choices made today will determine whether cutting-edge oncology tools will translate into far-reaching, equitable advances in patient care. There is an urgent need to invest in robust IT systems, rework reimbursement models, and ensure that every patient, regardless of their background or geographic location, has access to the therapies that can save lives.
This is not just a call for technological innovation—it is a call for human innovation, one that requires empathy, cooperation, and relentless dedication to ensuring that no one is left behind. The task ahead may be complicated and laden with twists and turns, but the potential benefits make it absolutely critical that we act now. The time has come to move beyond the limits of traditional practice and embrace a future where everyone has an opportunity to benefit from the best that modern oncology has to offer.
In concluding, let us remember that progress in medicine is measured not only by scientific breakthroughs but by how those breakthroughs improve lives. The road to equitable cancer care is certainly full of problems and nerve-racking challenges, but it is also filled with promise. With a united effort, we can build a system where every patient has a fighting chance, and every breakthrough is matched by fair access. We owe it to our communities, to our patients, and to the future of healthcare to make this vision a reality.
Originally Post From https://www.ajmc.com/view/no-outcome-without-access-delivering-on-the-promise-of-cancer-care-equity
Read more about this topic at
Access drives outcomes. In the Family Office world, deals …
The Texas OB/GYN Physician Workforce