Dynamic Gait Analysis and Meniscus Lesions: An Editorial Perspective
This editorial examines the recent study on gait characteristics in patients with meniscus lesions. The study, carried out at a renowned Sports Center in Chongqing, China, offers valuable insights by comparing the walking patterns of the affected versus the unaffected sides in individuals with confirmed meniscal injuries. By taking a closer look at the study’s methodology and results, we can better understand how dynamic gait analysis can shape early diagnosis, rehabilitation, and ultimately patient outcomes.
The use of dynamic, three-dimensional gait analysis in this field has provided clinicians and researchers with a novel window into the subtle, yet significant, differences in how patients walk when affected by a knee injury. This editorial will explore how this approach not only helps in pinpointing the tricky parts of meniscus injuries but also acts as a guide for developing personalized rehabilitation treatments.
Introduction: Skimming through Knee Injuries and Gait Dynamics
Knee injuries are one of the most common ailments that affect mobility, especially among active individuals. With the meniscus playing a crucial role in absorbing shock and stabilizing the knee, injuries in this area can be both intimidating and overwhelming for patients looking to make their way through recovery.
Recent research has indicated that careful analysis of gait—how we walk—can provide critical clues about the state of the meniscus. By comparing the affected side of the knee with the unaffected side, clinicians can spot early signs of dysfunction and take steps to prevent further complications. This study, therefore, offers a modern take on diagnosing and understanding the evolution of knee injuries.
Understanding the Study’s Methodology in Three-Dimensional Gait Analysis
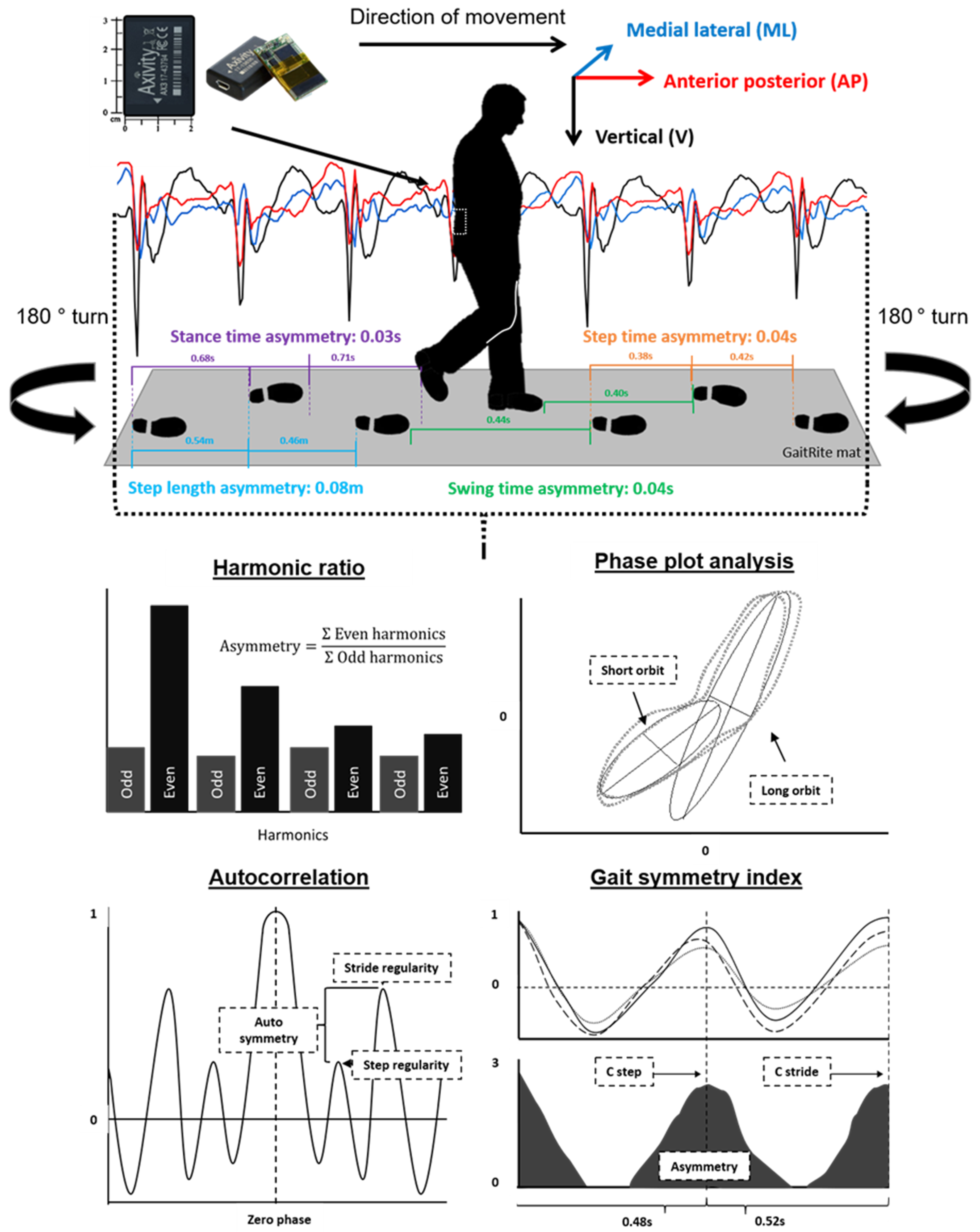
The study in focus involved 37 patients, each diagnosed with meniscus lesions confirmed by MRI and arthroscopic surgery. The researchers adopted a state-of-the-art Dynamic Gait & Posture Analysis System to analyze three-dimensional gait characteristics, comparing the affected and unaffected sides in detail. Such a rigorous, hands-on approach makes it possible to identify even the subtle details that might otherwise be overlooked.
Here are some key points about the methodology:
- Patient Selection: The study focused on a diverse group of individuals, both male and female, with varying durations of disease. This broad-based sampling helps in understanding how meniscus lesions affect different people.
- Technological Integration: Utilizing modern software and hardware for dynamic gait analysis provided a comprehensive look at how the affected side behaves while the patient ambles.
- Comparative Analysis: By directly comparing the affected and unaffected legs, the researchers could isolate the tiny twists and turns in gait that point to pain-avoidance strategies.
This detailed approach, using three-dimensional measurement tools, digs into the nitty-gritty of biomechanics. It helps us figure a path through the tangled issues that often come with knee injury diagnoses.
Key Findings: A Closer Look at the Propulsion Phase and Swing Velocity
The study’s findings introduce several intriguing observations about the gait of patients with meniscus lesions. One standout outcome is that patients demonstrated a notably shorter duration of the propulsion phase—the part of the walking cycle when the foot pushes off the ground—on the affected side compared to the unaffected side. This reduction appears to be a compensatory mechanism, possibly adopted to avoid pain.
In addition to the decrease in the propulsion phase, other dynamic parameters such as the velocity of impact, the maximum dorsiflexion velocity at the beginning of the swing (MDVBW), and the maximum swing velocity were all found to be significantly lower on the affected side. These findings suggest that patients subconsciously adjust their gait to minimize discomfort, adopting strategies that might lead to longer-term biomechanical imbalances if left unchecked.
To better illustrate these findings, consider the table below:
| Gait Parameter | Affected Side | Unaffected Side | Observation |
|---|---|---|---|
| Propulsion Phase Duration | Shorter | Longer | Indicative of pain-avoidance |
| Impact Velocity | Reduced | Higher | Reflects cautious movement |
| Maximum Swing Velocity | Lower | Higher | Suggests a protective gait strategy |
| MDVBW | Slower | Faster | Highlights diminished dynamic control |
These differences, while minor on the surface, offer a window into the subtle details of movement adaptation. The alterations in gait essentially represent a series of small distinctions that, when viewed collectively, allow healthcare professionals to take a closer look at the progression of knee pathology.
Implications for Early Detection and Treatment
The findings from the gait analysis hold promise for the early detection of meniscus injuries. One of the significant challenges in treating knee injuries is the delay in diagnosis. Often, by the time symptoms are severe enough for clinical evaluation, compensatory gait patterns have already set into motion, making rehabilitation a more tangled issue.
By teaching clinicians to spot these early signs—such as a reduced propulsion phase or slower impact velocities—dynamic gait analysis offers an essential tool for intervention. The early identification of side-to-side differences means that personalized rehabilitation plans can be established sooner, potentially curbing the progression of the injury.
Moreover, the integration of these findings into routine clinical practice can help demystify the confusing bits of knee pathology. Patients who undergo gait analysis can receive targeted therapies that focus on rebalancing their walking patterns, reducing the risk of future issues such as osteoarthritis.
Dynamic Analysis as a Key Tool in Rehabilitation
Modern rehabilitation strategies are increasingly relying on objective data to design patient-specific interventions. Dynamic gait analysis, with its comprehensive capture of walking metrics, is emerging as a key tool in modern rehabilitation—especially in cases of meniscal injuries.
This approach not only helps in tailoring rehabilitation exercises but also in monitoring progress over time. For example, if a patient’s gait begins to normalize after targeted therapy, it is a clear sign that the intervention is working. Conversely, persistent abnormalities may signal the need for an alternative course of treatment.
Rehabilitation programs designed with the help of dynamic analysis reduce the intimidating and overwhelming aspects of recovery. Patients gain clearer visibility into how each step is being improved, thereby making the process a much more manageable one. This data-driven approach underscores the critical need for objective monitoring in modern physical therapy.
Understanding Pain-Avoidance Patterns in Meniscus Lesions
Walking is such a routine activity that many of us rarely consider its mechanical complexity until we are forced to adjust because of an injury. In this study, the affected limb exhibited distinct pain-avoidance adaptations. Patients appear to reduce stance time during the propulsion phase and slow down their swing speed, likely to minimize discomfort caused by stressing the injured meniscus.
These behavioral modifications reflect the body’s natural inclination to protect an injured area. However, this strategy can come with its own set of problematic issues. Over time, relying on one side during ambulation can lead to further biomechanical imbalances, muscle weakness, and joint stress. Such side-to-side differences are a clear reminder of how the body compensates during pain and injury.
Identifying these subtle parts through dynamic gait analysis provides healthcare professionals with a roadmap for correcting these imbalances through targeted exercises and supportive therapies. Early intervention can make the difference between a complete recovery and chronic challenges in mobility.
Integrating Complementary Therapies with Modern Rehabilitation
In today’s healthcare environment, the integration of complementary therapies alongside traditional rehabilitation is gaining traction. While dynamic gait analysis offers a modern look at injury detection, merging it with alternative therapies such as acupuncture, mindfulness-based practices, and physical therapy can result in a more holistic approach to recovery.
For patients dealing with meniscal injuries, the combination of modern diagnostic techniques and complementary therapies can soften the nerve-racking process of physical recovery. For example, acupuncture may help alleviate pain and inflammation, while gentle, targeted exercises can rebuild stability and function. By working through these methods together, practitioners can not only mend the physical damage but also address the underlying biomechanical adjustments that have occurred due to pain avoidance.
It is essential that healthcare providers recognize the advantages of a multi-pronged approach. Complementary therapies can help move patients past the intimidating parts of physical rehabilitation, making the process more collaborative and less overwhelming. This fusion of modern and alternative methods underscores the value of taking a closer look at every aspect of patient well-being.
Challenges in Gait Analysis: Tackling the Tricky Parts and Tangled Issues
Despite the promising findings, gait analysis—especially in three dimensions—is not without its challenges. The field is loaded with issues regarding consistency in data capture, sensor placement, and individual variations in gait. Given that walking involves a series of repetitive motions, there is ample room for error, and even slight deviations in study setups can influence the results.
Some of the practical challenges include:
- Sensor Placement Accuracy: Ensuring that sensors are correctly placed to capture the fine points of gait is critical. Misplaced sensors can lead to data that is riddled with tension and may not accurately represent the patient’s true gait.
- Inter-Patient Variability: Every individual has a unique walking pattern influenced by age, weight, prior injuries, and even lifestyle. This makes it tough to set a standard baseline without considering these small distinctions.
- Data Interpretation: The dynamic nature of three-dimensional data collection means that clinicians must be equipped to interpret large volumes of information in a way that is both clear and actionable.
Addressing these tricky parts calls for continuous improvements in technology, standardized protocols, and better training for clinicians. By investing in these areas, the field of dynamic gait analysis can become even more robust and a reliable contributor to the early detection and treatment of meniscal injuries.
Future Directions: Innovative Techniques in Meniscal Injury Diagnostics
Looking ahead, the integration of artificial intelligence (AI) and machine learning with dynamic gait analysis promises to further refine diagnostic capabilities for meniscus lesions. AI algorithms could be trained to detect the subtle details and slight differences in gait patterns that might elude even experienced clinicians. This new era of innovation can help in three key areas:
- Automated Data Interpretation: With AI, large datasets can be processed in real-time, helping to quickly identify patterns that suggest early meniscal damage.
- Personalized Rehabilitation: Machine learning models can predict how individual patients are likely to respond to specific therapeutic interventions, allowing for more personalized treatment plans.
- Progress Monitoring: Continuous monitoring enabled by smart wearable devices could provide feedback to both patients and clinicians, ensuring that recovery protocols are tuned to the individual’s evolving needs.
These advances point toward an integrated future where dynamic gait analysis is part of a broader suite of diagnostic tools aimed at delivering a comprehensive understanding of knee mechanics. Such innovation is not only exciting but also a must-have for advancing the standards of care in musculoskeletal diseases.
The study we discussed is a stepping stone toward realizing this vision. As researchers and clinicians work together to figure a path through the tangled issues of meniscal injury, the future of knee diagnostics looks promising. The real challenge lies in incorporating these technological advancements while keeping the process accessible and understandable for both practitioners and patients alike.
Patient-Centered Implications and the journey to Better Mobility
From a patient’s perspective, understanding the reasons behind altered gait patterns following a meniscus injury can provide much-needed clarity and reassurance. The subtle changes in the propulsion phase and decreased swing velocity can be confusing bits of information that may be misinterpreted as signs of further deterioration.
When clinicians can effectively communicate what these changes mean—and how they tie into the overall healing process—it can significantly reduce the overwhelming nature of recovery. Patients are more likely to adhere to prescribed rehabilitation routines when they understand the rationale behind them and see tangible progress over time.
Furthermore, by embracing dynamic gait analysis, healthcare providers can better customize treatment plans. For example, if a patient’s affected limb shows a marked reduction in certain kinetic parameters, therapists might introduce exercises focused specifically on restoring those metrics. This targeted intervention not only helps in expediting recovery but also minimizes the risk of future injuries.
Patient engagement is super important in this process. When individuals are educated about the subtle parts of their condition, they are empowered to take better care of themselves. Beyond just physical therapy, understanding the interplay of pain-avoidance and dynamic adjustments can motivate patients to adopt lifestyle changes that further support their overall mobility and health.
Bridging the Gap Between Clinical Research and Everyday Practice
One of the most critical functions of contemporary research is to translate scientific findings into real-world applications. The study on gait characteristics in patients with meniscus lesions is an excellent example of how clinical research can shed light on everyday challenges faced by patients and guide clinicians in formulating better treatment strategies.
The integration of detailed dynamic gait analysis into routine orthopedic evaluations can bridge the gap between the laboratory and everyday clinical practice. By taking a closer look at the smaller distinctions in gait, healthcare professionals can move past the intimidating aspects of traditional diagnostics and embrace tools that offer nuanced data and actionable insights.
This bridging process involves not only the adoption of sophisticated technological tools but also the training of healthcare providers to interpret and apply this information effectively. Workshops, continuing medical education courses, and peer-reviewed publications all contribute to ensuring that the benefits of dynamic gait analysis reach as many patients as possible.
Encouraging Broader Adoption of Dynamic Gait Analysis
The potential benefits of dynamic gait analysis extend far beyond clinical research settings. When adopted more broadly, this technology can transform how we approach not only meniscal injuries but also other musculoskeletal disorders. For instance, early detection of subtle gait deviations could enable more proactive management of conditions such as osteoarthritis or chronic knee pain.
Adoption can be encouraged by highlighting these key advantages:
- Early Intervention: Detecting gait changes early can lead to timely interventions, reducing the risk of long-term joint damage.
- Tailored Rehabilitation: Customizing therapy based on precise data helps patients regain mobility faster, lessening the overall treatment time.
- Cost-Effectiveness: Although initial investments in technology may seem intimidating, the long-term savings associated with improved outcomes and reduced complications can be substantial.
Healthcare institutions, both large and small, should consider investing in these technologies as part of their routine diagnostic arsenal. As more clinicians get comfortable with interpreting the fine shades in dynamic data, the overall standard of care in musculoskeletal health will continue to improve.
Embracing a Future of Data-Driven Patient Care
In conclusion, the study of gait characteristics in patients with meniscus lesions underscores the transformative power of modern diagnostic techniques. By carefully comparing the affected and unaffected sides, researchers have not only highlighted behavioral adaptations to pain but also provided a roadmap for early intervention and improved rehabilitation strategies.
Dynamic gait analysis remains a promising frontier in the continuous effort to create more personalized, objective, and responsive patient care protocols. As the technology improves and integrates with artificial intelligence, we can expect even more refined data that will help clinicians dig into the small distinctions and subtle parts of movement. These insights are key to managing recovery and ensuring that patients make their way through rehabilitation with confidence.
For clinicians, researchers, and patients alike, the future looks bright. With data-driven approaches leading the charge, every step taken brings us closer to overcoming the tangled issues of knee injuries. Through collaboration, innovation, and a commitment to patient-centered care, dynamic gait analysis promises to remain a cornerstone of modern musculoskeletal diagnostics and treatment.
Conclusion: Advancements in Gait Analysis for Enhanced Patient Outcomes
This editorial has explored the multifaceted impact of dynamic gait analysis in understanding and treating meniscus lesions. One of the key takeaways is that even the seemingly minor side-to-side differences in gait can provide essential clues to the underlying health of the knee.
By working through the challenging elements of data interpretation and sensor placement, researchers are steadily making progress in unraveling the fine points of gait during walking. Healthcare providers who embrace these innovations are better positioned to design rehabilitation programs that are both effective and tailored to the individual needs of each patient.
Ultimately, the integration of modern diagnostic techniques with complementary and alternative therapies heralds a new era in musculoskeletal care. As we continue to figure a path through these confusing bits of data, the advancements made today are sure to pave the way for improved patient outcomes tomorrow. With an ever-evolving toolset at our disposal, dynamic gait analysis stands as a super important innovation that promises to reshape the landscape of knee injury rehabilitation and diagnosis.
The road ahead is filled with both challenges and opportunities. By staying at the forefront of technological and clinical advancements, the healthcare community can ensure that every patient receives personalized, efficient, and effective care. As we move forward, it will be critical to maintain open lines of communication between researchers, clinicians, and patients, ensuring that the exciting progress in dynamic gait analysis is translated into everyday clinical practice for the betterment of all.
Originally Post From https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1683174/full
Read more about this topic at
Comparative Gait Analysis Study Using Foot-Worn Inertial …
Comparison of gait analysis before and after unilateral total …