Transformative Shifts in Urologic Treatment Approaches
The field of urology is witnessing a rapid evolution that touches on several areas including bladder and kidney cancer, benign prostatic hyperplasia (BPH), and overactive bladder (OAB). With innovations coming thick and fast, urologists are now armed with a veritable arsenal of treatment options that offer patients more flexibility and a better quality of life. This opinion editorial takes a closer look at these advancements through the lens of clinical experience, discussing both the promising developments and the tricky parts associated with executing these new protocols.
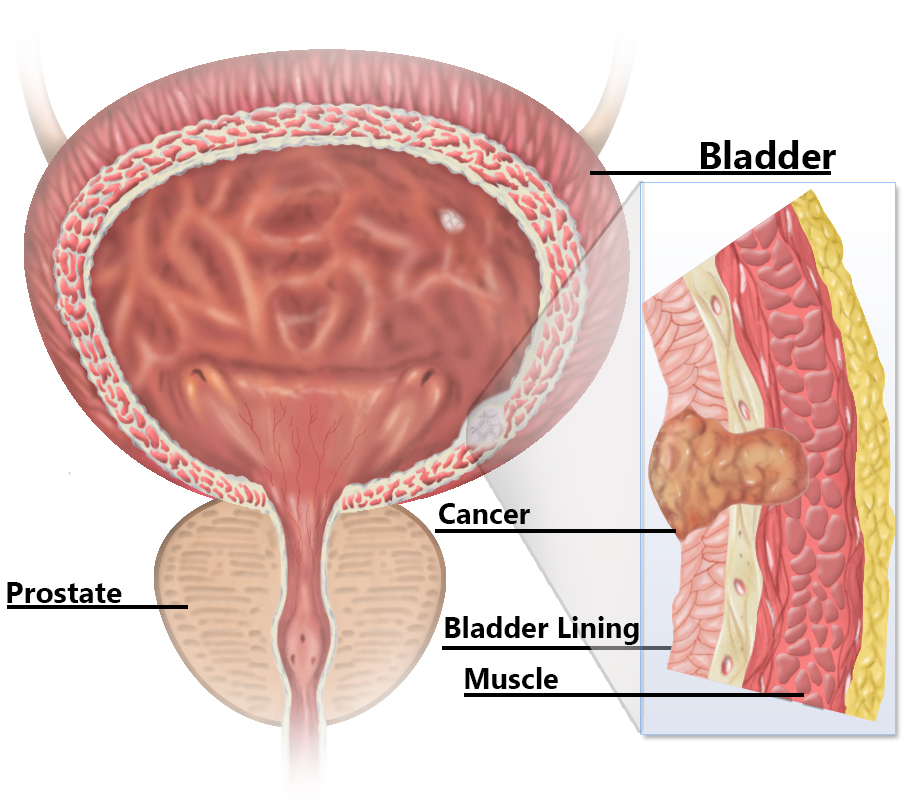
Recent progress in the management of non-muscle invasive bladder cancer (NMIBC) is particularly noteworthy. For years, the treatment landscape was considerably limited, leaving patients with little choice beyond BCG and, for some, an intimidating path toward radical cystectomy. Today, a range of alternative therapies has emerged, easing the pathway for both patients and practitioners.
Evolving Options for Non-Muscle Invasive Bladder Cancer
The journey to broaden treatment options for NMIBC has been marked by some tangled issues in the past. The widespread reliance on BCG often meant patients were caught in a nerve-racking cycle of shortage crises and limited alternatives. However, Dr. Elizabeth Mobley’s experiences—as shared at a major annual meeting—highlight an era in which urologists now enjoy what can only be described as an “embarrassment of riches.”
In the early days, many patients were forced to face a radical cystectomy if they failed initial treatments such as BCG. This was not only intimidating but also laden with numerous post-operative challenges. As newer agents emerged—such as Adstiladrin (nadofaragene firadenovec), Anktiva (nogapendekin alfa inbakicept-pmln), and Inlexzo (a gemcitabine intravesical system)—they provided new ways to manage this condition without resorting to such drastic measures.
The key benefits of these alternatives include:
- Flexible dosing options that help avoid the rigid schedules once imposed by frequent maintenance regimens.
- Improved accessibility for patients who travel long distances, as some treatments now demand only quarterly administration rather than multiple visits in a few weeks.
- Expanded treatment protocols that allow the assessment and adjustment of therapy based on individual patient needs.
This evolution mirrors the broader trend in modern healthcare of striving for more personalized, patient-centered care. Having multiple tools available not only gives patients hope but also supports urologists in crafting treatment plans that consider the fine points of each case. While the introduction of these new treatments comes with its own set of challenges—particularly in managing cost and insurance coverage—the overall benefits are undeniable.
Refined Techniques in Muscle-Invasive Bladder Cancer Management
Muscle-invasive bladder cancer (MIBC) represents a stage where treatment decisions have long been full of problems and unpredictable outcomes. The latest data from landmark studies such as the NIAGARA and KEYNOTE-905/EV-303 trials are now shifting paradigms in this area. In these studies, perioperative immunotherapy combined with chemotherapy is proving to be a game changer, potentially setting a new standard of care.
One major development in this space is the introduction of circulating tumor (ctDNA) testing. This technology helps clinicians figure a path through the maze of adjuvant treatment decisions by identifying which patients might benefit from continued immunotherapy. With ctDNA testing, rather than relying solely on traditional risk factors, urologists now have a tool that digs into the small distinctions that make each patient’s case unique.
Dr. Mobley emphasizes that while she involves medical oncologists early in the treatment process for MIBC, the incorporation of these data-driven, immunotherapy-based protocols is reshaping how referrals are made and how treatments are planned. With ctDNA testing guiding decisions on adjuvant therapy, the process becomes less nerve-racking for patients and helps tailor treatment so that only those who need additional therapy are subjected to more intensive regimens.
The potential benefits of this approach include:
- Reductions in over-treatment and the corresponding side effects from unnecessary chemotherapy or immunotherapy.
- Enhanced ability to personalize treatment plans, which accounts for the subtle parts unique to each patient’s cancer biology.
- A promising future where bladder-sparing techniques may emerge as a preferred option in select cases.
This shift is a testament to the ongoing attempts by the medical community to sort out the confusing bits of treatment standards in a manner that best suits patient needs. While challenges such as insurance approvals and managing new side effects remain, the overall trend is one of cautious optimism and rapidly evolving best practices.
Advancements in Kidney Cancer: Keeping Care Under One Roof
Kidney cancer treatment has equally benefited from the wave of modern therapies focusing on immunotherapy. One innovative strategy has been the establishment of in-house infusion centers by urologic groups. This development not only simplifies logistics for patients but also allows them to continue receiving care from specialists they know well—a crucial factor when dealing with what might otherwise be an overwhelming treatment journey.
In these dedicated centers, treatments like pembrolizumab (Keytruda) are administered, ensuring that patients with locally advanced kidney cancers receive timely and integrated care. Dr. Mobley’s team, for instance, embraced the challenge of setting up such an in-house infusion center. Although taking the first step was obviously nerve-racking, it ultimately provided a safe and convenient environment for patients, demonstrating how coordinated care can deliver top-notch outcomes.
Here are some key benefits observed with this integrated approach:
- Continuity of Care: Patients remain under the care of their trusted urologist, easing the transition between surgery and subsequent treatment phases.
- Reduced Exposure to Hospital Settings: By managing immunotherapy within a familiar outpatient facility, patients can avoid the added stress of navigating a separate oncology department.
- Rapid Response to Side Effects: With a specialized team including medical oncology, gastroenterology, endocrinology, and dermatology on hand, the little twists and turns of adverse events can be managed more promptly and effectively.
This approach also underscores the importance of keeping an open dialogue with patients regarding the potential side effects and the importance of reporting any unexpected symptoms early. While managing immunotherapy side effects can be complicated, having a multidisciplinary team means that these issues—though any patient might find them a bit intimidating—are addressed quickly.
Innovations in BPH Management: Tailored Treatments for Individual Needs
Benign prostatic hyperplasia (BPH) is another condition that has seen significant improvements in treatment options in recent years. Within this arena, the focus has shifted to minimally invasive therapies that provide relief while preserving overall bladder health—a super important factor for long-term urinary function.
Dr. Mobley’s practice, for example, now offers cutting-edge treatments such as the UroLift system, iTind, and Aquablation. Each of these procedures targets the prostate in a distinct manner:
- UroLift: Uses implants to retract the prostate tissue, effectively widening the urethral passage without cutting tissue.
- iTind: A temporary implant that reshapes the prostate and relieves urinary symptoms in a minimally invasive way.
- Aquablation: A robotic, waterjet-guided procedure that precisely removes the obstructive prostate tissue while being highly reproducible and quick—with most procedures lasting an hour or less.
Each option is chosen based on careful work-ups that include diagnostic cystoscopy, ultrasounds, flow studies, and sometimes urodynamic testing. This detailed evaluation helps drive home the key importance of preserving bladder health, as untreated BPH can cause subtle long-term changes in the bladder’s function.
A typical diagnostic table employed in the work-up process might look like this:
| Test | What It Assesses | Impact on Treatment Selection |
|---|---|---|
| Cystoscopy | Urethral integrity, prostate anatomy, bladder neck | Helps decide if procedural intervention is safe |
| Ultrasound | Prostate size and shape | Assists in matching the patient with suitable treatments |
| Urinary Flow Testing | Flow dynamics and degree of obstruction | Determines severity and guides choice between medication and procedure |
| Urodynamic Studies | Bladder function and detrusor muscle performance | Influences decisions especially when symptoms are variable |
This meticulous, data-driven process ensures that treatment is precisely matched to each patient’s needs. While the range of options is exciting, the process of matching the right treatment to the right patient involves managing subtle details and is not without its challenges. The work of sorting out these little details forms the backbone of effective BPH management, one that ultimately prioritizes a patient’s long-term well-being over short-term fixes.
Overactive Bladder (OAB): Striking the Balance Between Guidelines and Insurance Realities
Overactive bladder (OAB) remains a challenging condition in urology. Although recent guideline updates from leading urological associations provide comprehensive options for early procedural interventions, the reality on the ground is often quite different. Insurance companies, for example, may not readily align with the new guidelines, forcing both patients and physicians to work through a maze of approvals and requirements.
The challenge here is twofold. On one hand, clinicians have an expanded toolkit that includes options such as neuromodulation, onabotulinumtoxinA (Botox) injections, and implantable tibial nerve modulators. On the other hand, many patients find themselves caught in the confusing bits of insurance policies that still require the failure of one or two drug therapies before they will approve these newer procedures.
This division between clinical flexibility and insurance restrictions creates some tricky parts. Patients are often advised to try oral medications—beta-3 agonists, for instance—despite their sometimes off-putting side-effect profiles. While these medications can offer relief, they are particularly problematic in older patients where anticholinergics might carry an increased risk profile.
What’s necessary, therefore, is better alignment between clinical guidelines and payer practices. Until then, urologists will continue fighting the battle on behalf of their patients, striving to secure the procedures that promise better long-term outcomes, such as less risk of adverse drug reactions and improved bladder function.
The pathway for many patients with OAB involves:
- Initial conservative management with lifestyle modifications.
- Medication trials, which often prove to be just the beginning.
- Procedural interventions when indicated, although these are sometimes delayed due to reimbursement issues.
It is clear that a major improvement in insurance policies is critical to higher rates of procedural intervention. With patients often suffering in silence due to both the physical discomfort and the social stigma of their symptoms, expanding access to effective treatments must be a priority in the coming years.
Integrating Multidisciplinary Care: A New Standard for Urologic Practice
What truly makes these advances exciting is not just the technological progress alone, but also the ability to integrate care across multiple specialists within the same healthcare setting. Whether it’s through the incorporation of in-house infusion centers for immunotherapy or closer collaborations with oncologists, endocrinologists, and other specialty colleagues, modern urology is becoming a multidisciplinary endeavor.
This collaborative approach has several advantages:
- Smoother transitions between treatment phases: With all stakeholders working together, patients experience fewer delays and less confusion during the treatment process.
- Enhanced capacity to manage side effects: The presence of experts from various fields helps address the little twists and turns that sometimes come with innovative therapies.
- Increased patient confidence: Knowing that a dedicated team is working together under one roof often reassures patients and encourages adherence to treatment protocols.
The benefits of an integrated care model cannot be overstated, particularly for complex conditions like kidney cancer and muscle-invasive bladder cancer where managing treatment side effects and complications demands knowing one’s way around a multifaceted medical system. As the field of urology continues to push boundaries, multidisciplinary practices stand out as an ideal framework for managing both new treatment modalities and the associated challenges.
Personalized Treatment: The Role of Patient-Centered Approach in Modern Urology
At the heart of all these advancements is a renewed commitment to personalized, patient-centered care. Gone are the days when a one-size-fits-all approach was acceptable. Today, the focus is on engaging patients in the decision-making process from the outset, ensuring they are well-informed about their options, the potential benefits, and the possible side effects of each treatment route.
For example, when discussing BPH treatments, it is not uncommon for a clinician to frame the conversation around the idea that “the prostate at this stage of life is more of a hindrance than a helper.” By explaining the long-term impact of bladder outlet obstruction on bladder function, patients are better able to appreciate why early intervention might be necessary. The process usually begins with a detailed work-up that may include cystoscopy, various imaging studies, and flow tests. Armed with this objective data, the urologist and patient can work together to choose a intervention that not only treats the symptoms but also preserves the bladder and overall urinary tract health.
This approach is critical because it ensures that treatment decisions are made after taking into account the fine shades that differentiate one patient’s experience from another’s. It is only by engaging deeply in these conversations that both patients and physicians can find their way through the maze of available options, weigh the pros and cons of each therapy, and ultimately select the most appropriate treatment pathway.
Addressing the Insurance Hurdles: A Call for Policy Reform
A recurring theme in modern urologic care is the problem of insurance coverage. Although clinical guidelines have evolved to endorse earlier procedural interventions for conditions like OAB and BPH, many insurance policies remain on edge, clinging to outdated criteria that delay access to these innovative treatments.
For many patients, the process of obtaining coverage for a procedure can feel like a nerve-wracking hurdle filled with bureaucratic tangles. This disconnect between best clinical practices and insurance policies is a prime example of how policy reform must catch up with medical innovation. It is essential for practitioners to work with policymakers and payers to create coverage policies that are in line with current treatment guidelines—not only to speed up care but also to reduce the unnecessary suffering of patients.
Some potential solutions include:
- Revising coverage criteria to allow for earlier procedural intervention based on updated guidelines.
- Encouraging pilot programs that test the effectiveness of these newer treatments under real-world conditions, thereby providing evidence for broader insurance acceptance.
- Establishing more robust communication channels between healthcare providers and insurance companies to discuss the clinical benefits of innovative treatments.
The ultimate goal is to reduce the small distinctions between what is medically optimal and what is actually accessible to patients under current insurance frameworks. Without such changes, even the best technological and therapeutic advances could fail to realize their full potential in improving patient outcomes.
The Road Ahead: Embracing Change in Urologic Practice
Looking forward, it is clear that almost every facet of urologic care is undergoing a transformation. With significant progress in the management of both cancerous and benign urologic conditions, the future appears promising, yet is not without its complicated pieces. Clinicians, patients, and policymakers alike must work together to ensure that the benefits of modern treatments reach every individual in need of care.
Key areas for future growth include:
- Enhanced Diagnostics: Continued refinement and wider adoption of tests such as ctDNA can further tailor adjuvant treatment approaches, minimizing risks and maximizing efficacy.
- Broadened Access: Efforts to simplify the process of in-house care, like infusion centers, and to ease insurance approvals, will democratize advanced kidney cancer and bladder cancer treatments.
- Multidisciplinary Care Models: By fostering closer collaborations between various specialties, urologic practices can manage side effects more effectively and ensure a smoother patient journey.
- Patient Education and Engagement: Investing in patient education initiatives to help individuals understand the fine details behind their treatment options will facilitate a more open and reassuring dialogue between patients and providers.
It is essential that clinicians remain active in clinical trials and research, helping to refine and validate emerging therapies. This not only addresses the hidden complexities within each treatment modality but also plays a super important role in setting the stage for next-generation urologic care. The innovations we see today are just the beginning; tomorrow’s breakthroughs will build on these foundations, further demystifying what was once seen as an overwhelming landscape of treatments.
Charting a Path Forward in a Time of Rapid Change
Every transformation in medicine carries with it a set of small distinctions and subtle challenges. The rapid evolution in urologic care—whether it concerns the adoption of immunotherapy for muscle-invasive bladder cancer or the integration of minimally invasive techniques for BPH—demands that clinicians keep an eye on both the promise of new treatments and the very real hurdles of their implementation.
In many ways, the current era in urology can be likened to working through a series of interlocking puzzles, where each new advancement is a piece that must fit seamlessly into the patient’s overall treatment plan. For example, clinicians must figure a path through the combination of advanced cancer treatments, improvements in benign disease management, and the practicalities of insurance-mediated access to care.
A few practical steps to bolster this journey include:
- Maintaining open communication with patients regarding their evolving treatment options.
- Collaborating closely with insurance providers to better align policies with modern clinical practices.
- Continuously updating the clinic’s technological and clinical protocols to integrate the latest research and trial data.
- Participating in and supporting clinical trials that help map out the effectiveness and safety profiles of new treatments.
It is through such consistent, patient-centered efforts that the urology community can ensure that no one is left behind. Each positive outcome not only boosts patient confidence but also contributes meaningfully to the broader shift toward more tailored, effective, and compassionate care.
Embracing a New Era With Confidence and Compassion
The remarkable strides being made in urology speak to a larger trend in medicine: a move away from one-dimensional treatment plans toward a more nuanced, multidisciplinary approach that considers the individual patient’s entire journey. This change is not without its nerve-wracking challenges—ranging from insurance hurdles and logistical issues to managing immune-mediated side effects—but the promise of greater efficacy and improved quality of life is a prize worth striving for.
Clinicians are increasingly finding that by working together, they can create streamlined processes that permit patients to receive advanced therapies without the added stress of additional referrals or fragmented care. With innovations like flexible dosing schedules, in-house infusion centers, and minimally invasive procedures, the strides being made are both significant and encouraging.
Moreover, the integration of patient education into these advanced treatment pathways ensures that patients are not left in the dark. Instead, they are active, informed participants in their care—a shift that has proven to yield better outcomes overall. When patients understand the little twists and turns of their treatment journey, from the subtle details in diagnostic tests to the specific benefits of modern therapies, they are more likely to adhere to treatment protocols and achieve optimal results.
Conclusion: Partnering for a Healthier Future in Urology
In summary, the current state of urologic care is as dynamic as it is promising. From the expanded repertoire of treatments for non–muscle invasive bladder cancer to the integrated, in-house management of kidney cancer, and from the innovative minimally invasive solutions for BPH to the ongoing challenges in OAB treatment, it is clear that modern urology is thriving on innovation and patient-centered progress.
At its core, the evolution we observe today is a reflection of the relentless drive for better patient outcomes—a drive that requires both technical advancement and the readiness to figure a path through the confusing bits of administrative and clinical challenges. With ever-improving diagnostic tools, personalized treatment plans, and a collaborative, multidisciplinary approach, urology is well poised to face the future.
As clinicians and healthcare providers, the journey ahead is about more than just adopting new technologies—it’s about embracing change with confidence and compassion. By continuing to push through the twists and turns of evolving treatment protocols, we can ensure that our patients receive not only the most advanced medical care available but also the thoughtful, individualized approach they deserve. While navigating these changes is never simple, it is through persistence, innovation, and cooperation that the field of urology will continue to thrive, guiding us toward a healthier future for all patients.
Originally Post From https://www.urologytimes.com/view/urologist-elizabeth-mobley-md-discusses-advances-in-bladder-and-kidney-cancer
Read more about this topic at
Revolutionizing Patient Care in Urology with New …
How Technology Is Revolutionizing Urology

