Virginia’s Lung Cancer Challenge: Progress and Persisting Obstacles
The fight against lung cancer in Virginia has seen both encouraging improvements and lingering concerns. A recent report by the American Lung Association shines a light on the progress made, while at the same time reminding us of the many tangled issues that still need addressing. In this opinion editorial, we take a closer look at the advances in diagnosis and treatment, the tricky parts of ensuring widespread screening, and the legislative measures that could potentially enhance patient outcomes across the state.
As we consider the impact of lung cancer on communities throughout Virginia, it is important to recognize not only the statistically significant gains in reducing the number of new cases but also the nerve-racking delays in early detection. The report reveals that Virginia has improved its ranking and performance in several metrics relative to lung cancer care, yet the percentage of eligible individuals receiving screening is still far from ideal. With lung cancer continuing to be a leading cause of cancer deaths, we cannot afford to overlook any aspect of its management.
Examining Recent Improvements in Lung Cancer Incidence
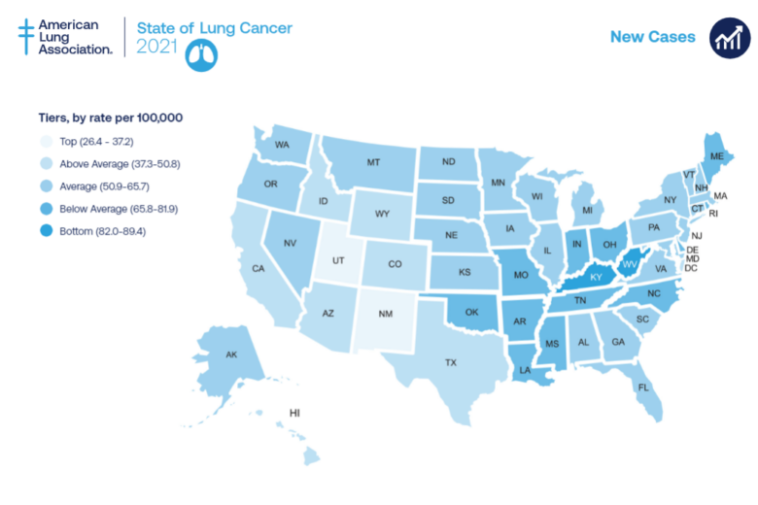
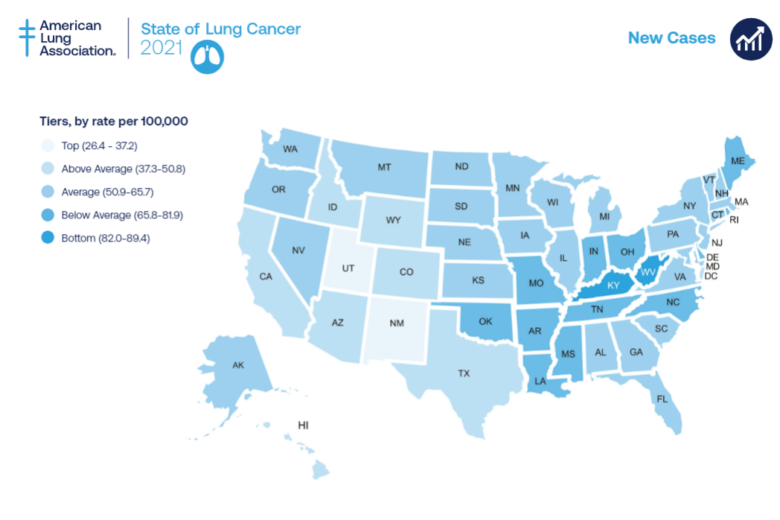
One of the report’s central takeaways is that Virginia has experienced about an eight percent improvement in new lung cancer cases over the past five years. Ranking 17th in the nation for new cases, Virginia has made strides that show promise, especially when it comes to treatment outcomes. The report places the Commonwealth fourth among states with the lowest percentage of patients not receiving proper care—a statistic that highlights the effectiveness of current treatment protocols.
However, such improvements mask the underlying challenges. The progress made is significant, yet it has come with its own set of twists and turns. While the reduction in incidence suggests that prevention initiatives and improved healthcare interventions are making a difference, these gains are counterbalanced by the persistent issues of delayed diagnosis and lack of routine screenings. It is this dual reality that sets the stage for a more comprehensive discussion on how to move forward in our battle against lung cancer.
Improving Early Detection of Lung Cancer with Biomarker Testing
Early detection is one of the key pillars in reducing lung cancer mortality. However, the report underscores that only about 18.2 percent of people eligible for screening nationwide are actually getting screened. In Virginia, the numbers are just slightly above the national average at around 18.4 percent. This marginal difference demonstrates that despite progress in treatment outcomes, the early identification of the disease remains a significant challenge.
Biomarker testing has emerged as a super important tool in this scenario. It allows oncologists to gain a better understanding of the individual characteristics of a patient’s cancer, which in turn helps in choosing the most effective treatment strategies. Expanding the availability of such tests, along with routine screenings, could make a big difference in catching the disease before it advances into a more complicated, nerve-racking stage.
- Biomarker testing provides insights into the biological makeup of lung tumors.
- It helps tailor treatments to each patient’s specific needs.
- Early detection through biomarker testing raises survival rates significantly.
Legislation and Policy: Essential Strategies to Enhance Early Detection Capabilities
Legislation plays a crucial role when it comes to making critical healthcare interventions more accessible. The American Lung Association has urged Virginia lawmakers to consider mandating insurance coverage for biomarker testing. Such policy initiatives could pave the way for a broader adoption of early detection practices, ensuring that more patients have access to testing that can identify lung cancer in its initial stages.
This kind of policy change is not just bureaucratic maneuvering—it represents a key, actionable step forward. By addressing the tangled issues of varying insurance coverage and inconsistent testing standards, legislators can help steer through the confusing bits that currently hinder effective lung cancer diagnosis.
In practical terms, policymakers might consider the following actions:
| Action | Potential Impact |
|---|---|
| Mandating insurance coverage for biomarker testing | Increases early detection rates and individualizes treatment |
| Funding public health campaigns | Raises awareness about the importance of lung cancer screening |
| Incentivizing healthcare providers | Encourages more proactive testing and comprehensive care |
| Improving data collection and sharing | Enables a clearer picture of lung cancer trends in Virginia |
Looking Deeper into the Role of Biomarker Testing for Treatment Personalization
Biomarker testing is not only about early diagnosis but also about customizing patient treatment plans. By identifying the specific markers or genetic mutations that drive lung cancer, doctors can select treatments that are more likely to be effective for individual patients. This approach enables tailored therapy, reducing the number of trial-and-error treatments and potentially lessening the overall burden of the disease.
Many healthcare providers are beginning to see the benefits of this personalized medicine approach. However, making these advanced tests available on a wide scale remains an intimidating challenge, particularly in under-resourced communities. The benefit is clear: improved outcomes, better quality of life for patients, and a more direct impact on survival rates. Despite these advantages, issues with accessibility—such as cost, insurance hurdles, and limited availability—continue to pose problems that require decisive action from both medical professionals and legislators.
Some of the fine points contributing to the success of biomarker testing include:
- Enhanced treatment matching based on a patient’s unique cancer profile
- Reduction in the use of broad-spectrum treatments that may be less effective
- Potential for improved overall survival rates
- Greater patient satisfaction and confidence in their treatment plan
Identifying Tricky Parts in Advancing Lung Cancer Screening Programs
The statistics clearly point out that the current level of lung cancer screening is not sufficient. Despite improvements in treatment, the fact that less than one-fifth of eligible individuals receive screening indicates a significant gap. This gap is riddled with tension, driven by several interdependent factors, some of which include public awareness, logistical issues, and the cost of screening tests.
For many, deciding to get screened can feel like a nerve-racking process. The path from recognizing subtle symptoms to undergoing comprehensive testing is filled with little twists and confusing bits. Public health officials must work to ease these obstacles by providing clear, accessible information about the screening process, as well as offering support and resources to guide individuals through this critical step.
A combination of educational campaigns, improved outreach, and community-based initiatives could help demystify the screening process. Some of the necessary steps to boost screening rates are:
- Community health workshops and public seminars
- Enhanced communication from healthcare providers
- Accessible and affordable screening options
- Proactive follow-up procedures for those identified as high-risk
A Comparative Analysis: Virginia Versus Other States in Lung Cancer Management
When comparing Virginia’s lung cancer metrics with those of other states, it becomes clear that while the Commonwealth has made noteworthy improvements, the overall picture remains mixed. Virginia’s rank of 17th for new lung cancer cases is impressive when considered alongside its superior treatment outcomes—ranking fourth for the lowest rate of untreated patients. Yet, the early detection statistics leave much to be desired.
This comparative analysis draws attention to areas where Virginia excels and those where it lags behind. For instance, states with more aggressive screening programs and robust insurance policies covering biomarker testing tend to report higher early detection rates and, consequently, better survival outcomes. It is a reminder that progress in one area does not automatically translate to overall success if other critical components are not addressed.
Below is a simplified table that summarizes how Virginia compares to other states in key lung cancer indicators:
| Indicator | Virginia | Leading States |
|---|---|---|
| New Lung Cancer Cases | 8% improvement over five years | Varies, but generally lower incidence rates |
| Treatment Outcomes | 4th lowest percentage of untreated patients | Top three in some cases |
| Screening Rates | Approximately 18.4% | Varies widely; some states exceed 25% |
This snapshot not only shows Virginia’s current status but also highlights the nerve-racking gaps that exist when compared with the best-performing states. Bridging this gap will necessitate a multi-faceted approach involving policy reform, increased investment in public health initiatives, and a commitment to patient education.
Future Directions: Expanding Access and Improving Survival Rates
The path forward for Virginia’s lung cancer management is both promising and challenging. The potential for expanding access to essential screening tests and biomarker assessments could transform outcomes for countless patients. For many, the opportunity to have early detection means not only a better chance at survival but also a higher quality of life during and after treatment.
Key future directions include:
- Increasing Public Awareness: Many individuals are unaware that they are eligible for lung cancer screening. Enhanced public education campaigns can help demystify the process, reduce fears, and encourage routine testing.
- Streamlined Healthcare Access: Simplifying the process of getting screened can alleviate the overwhelming journey for patients. This includes reducing bureaucratic steps and ensuring proper follow-up care.
- Expanding Insurance Coverage: Legislative initiatives that mandate insurance coverage for biomarker testing and routine lung cancer screenings can play a significant role in improving early diagnosis.
- Investing in Technology and Training: Equipping healthcare providers with updated diagnostic technologies and training is essential for identifying lung cancer at its most treatable stage.
By taking these steps, Virginia can work toward a future where the early detection rate is no longer a stumbling block, but rather a cornerstone of an effective lung cancer management program.
Actionable Steps and Recommendations for Policy Makers and Healthcare Providers
In order to truly turn the tide in Virginia’s lung cancer battle, a coordinated effort is required. This involves collaborating across multiple sectors—from government and healthcare institutions to community organizations and patient advocacy groups. Here are some actionable recommendations:
- Enhance Legislative Support: Policymakers should push for laws that require full insurance coverage of biomarker tests and regular lung cancer screenings for at-risk populations. Such measures would help reduce the tangled issues of cost and accessibility.
- Implement Community Outreach Programs: Local health departments and community organizations can take the wheel by organizing events that educate people about the importance of early detection and how to get screened. These programs should also address the nerve-racking fears associated with the screening process.
- Upgrade Healthcare Infrastructure: Investing in state-of-the-art diagnostic equipment and training for healthcare personnel can ensure that even the subtle, little details of lung cancer symptoms are not missed. This includes making sure that biomarker testing is widely available.
- Create Incentives for Healthcare Providers: Financial and professional incentives can encourage providers to actively recommend and facilitate lung cancer screenings. Recognizing and rewarding achievements in early diagnosis could motivate a broader adoption of best practices.
- Boost Data Collection and Sharing: Establishing a comprehensive database that tracks lung cancer cases, screening rates, and treatment outcomes will provide valuable insights. This information can guide future interventions and help identify areas that need improvement.
Each of these recommendations addresses a specific tricky part in Virginia’s healthcare system. While some issues are complicated pieces that have been persistent over time, others are more directly solvable through targeted legislative and healthcare initiatives. The overall message is clear: with coordinated effort and continued investment in early detection measures, Virginia has the potential to become a model for lung cancer management.
Community Engagement and Public Health: Turning Statistics into Lives Saved
Data and statistics, though critical, represent only one side of the lung cancer story. Behind every percentage is a person—a parent, a friend, or a coworker—who has to navigate the daunting and intimidating reality of a cancer diagnosis. Effective public health campaigns that tie these statistics back to personal stories can have a profound impact on community engagement.
Consider the following bullet points as essential elements in transforming awareness into action:
- Personalized Messaging: Stories from survivors and families can help demystify the screening process and reduce the off-putting fear associated with a diagnosis.
- Localized Health Initiatives: Community-based programs that align with local values and cultural practices can encourage more people to get screened.
- Partnerships with Local Leaders: Doctors, community leaders, and educators can work together to disseminate reliable information and support screening initiatives.
- Interactive Health Fairs: Events where residents can ask experts questions, participate in basic screening simulations, and receive guidance on next steps can turn the abstract statistics into tangible, life-saving action.
Ultimately, it is this human connection that underpins the technical progress in lung cancer management. When community members are well-informed and engaged, they are more likely to take responsibility for their health and participate in screening programs that can catch the disease early.
Barriers to Routine Lung Cancer Screening and How to Overcome Them
Despite the clear benefits of early detection, several barriers continue to restrict routine lung cancer screening. These barriers are loaded with issues that range from logistical challenges to cultural misunderstandings and economic constraints. Overcoming these barriers requires a multifaceted approach, as outlined below:
- Cost Concerns: The direct and indirect costs associated with screening make it a less-than-ideal option for some individuals. Subsidized programs and financial assistance can help lower this burden.
- Limited Access to Testing Facilities: Particularly in rural areas, the availability of modern diagnostic tools is often limited. Mobile screening units and telemedicine services can help bring these essential services to remote communities.
- Lack of Awareness: Many eligible individuals do not know they should get screened. Educational campaigns, supported by community health workers, can spread the word and ensure that the message reaches every corner of the state.
- Fear and Anxiety: Undergoing screening or awaiting results can be intimidating. Providing clear information on what to expect and ensuring that mental health support is available can mitigate these nerve-racking feelings.
Addressing these barriers is not only important for increasing screening rates but also for building trust between healthcare providers and the communities they serve. Every initiative aimed at reducing these obstacles is a step toward saving more lives and improving overall public health.
Turning Policy into Practice: The Role of Local and State Governments
The potential for policy reforms to reshape lung cancer management in Virginia is immense. Local and state governments have a super important role to play in turning policy ideas into practical, everyday reality. Here are some ways in which government action can directly influence the fight against lung cancer:
- Enhanced Funding: Allocating funds specifically for lung cancer research, screening programs, and patient support services can drive overall improvements.
- Regulatory Support: Regulations that require timely and routine screening for high-risk groups can make a direct impact on early detection statistics.
- Public-Private Partnerships: Collaborations with private healthcare companies and non-profit organizations can help spread costs and share successful strategies across multiple sectors.
- Data Transparency: Keeping the public informed about lung cancer trends and progress builds trust and encourages community involvement.
In addition, local governments can tailor their approach by focusing on the unique challenges their communities face. Whether it’s limited access to healthcare facilities or cultural barriers to routine screening, region-specific policies can help overcome these challenges more effectively than a one-size-fits-all approach. In this manner, government action acts as a critical catalyst for turning broad policy goals into concrete, life-saving practices.
Reflections on the American Lung Association’s Report and Its Broader Implications
The recent report by the American Lung Association serves as both a milestone and a wake-up call. While it celebrates the progress Virginia has made—in terms of reducing new lung cancer cases and improving treatment metrics—it also highlights significant gaps in early detection. The realities laid out in the report call for a deeper, more concerted effort to improve screening rates and healthcare accessibility.
In essence, the report is a reminder that while data and statistics are instrumental in understanding progress, the real-world implications impact lives. The slight improvement in early detection numbers is not enough to quell the growing concern; much work remains to get around the nerve-racking challenges facing early diagnosis.
For medical professionals, legislators, and community advocates, the report emphasizes the need to:
- Dig into the root causes limiting early screening rates.
- Understand the fine points of biomarker testing and its benefits for personalized treatment.
- Address the economic and social barriers that leave many vulnerable.
Through a concerted, community-driven effort, Virginia can overcome these tricky parts, ensuring that every individual at risk has access to the life-saving screening and treatments they need.
Building a Roadmap for Enhanced Lung Cancer Management in Virginia
As we look to the future, it becomes clear that a strategic, multi-pronged approach is necessary to maintain the gains made in lung cancer management while addressing its remaining challenges. A collaborative roadmap might include the following steps:
- Strengthen Community Engagement: Establish recurring community workshops, health fairs, and public seminars focused on lung cancer awareness and screening benefits.
- Invest in Medical Infrastructure: Allocate resources to boost the availability of advanced diagnostic tools and ensure that healthcare facilities, especially in rural areas, are well-equipped.
- Optimize Data Usage: Make use of state-wide health data to identify high-risk zones and deploy targeted interventions, ensuring that efforts are both efficient and impactful.
- Enhance Training and Support: Provide continuous professional development for healthcare providers around the latest techniques in biomarker testing and personalized treatment planning.
- Create Policy Incentives: Encourage partnerships between the public and private sectors through incentives that bolster research and lower the costs of critical diagnostic methods.
When communities, clinicians, and policymakers work together, navigating the confusing bits and subtle details of healthcare becomes a shared responsibility. This kind of integrated approach not only addresses the immediate challenges but also builds a resilient system capable of adapting to future changes and obstacles.
Conclusion: A Call for Collaborative Action in the Fight Against Lung Cancer
Virginia’s journey in combatting lung cancer presents a picture that is both hopeful and cautionary. On one hand, significant strides have been made in reducing new cases and ensuring that treatment is increasingly accessible and effective. On the other hand, the low rates of early detection and the lingering challenges associated with screening signal that there is still a long way to go.
This opinion editorial underscores the importance of turning data-driven insights into practical, community-based actions. By expanding access to biomarker testing, enhancing legislative support, and actively working through the tricky parts of patient engagement and healthcare accessibility, Virginia can continue to improve outcomes for lung cancer patients.
It is essential for all stakeholders—healthcare providers, policymakers, community advocates, and patients themselves—to get into a dialogue, share responsibilities, and take decisive steps. The progress reported by the American Lung Association is a stepping stone, not the final destination. To truly honor the advancements achieved so far, Virginia must commit to addressing the remaining challenges head-on.
In the end, the story of lung cancer in Virginia is not just about statistics or reports—it’s about people. Every increase in early detection and every improvement in treatment outcomes represents a life saved, a family kept whole, and a community that is stronger for its efforts. As we face the confusing bits, tricky parts, and nerve-racking hurdles of lung cancer management, let us remember that every step we take toward better screening and treatment is a step toward a healthier, more resilient future for all.
Now is the time for actionable change. It is super important that legislative reforms, improved access to healthcare, and community-level awareness efforts come together. By doing so, Virginia can continue to serve as a model of progress while ensuring that each person has the chance to reclaim their health and live a fulfilling life free from the devastating grips of lung cancer.
This call for collaborative action is not merely an editorial opinion—it is a critical appeal for a united approach across all sectors of society. Whether through pushing for policy reform, investing in healthcare innovation, or simply spreading the word about the benefits of early detection, every effort counts. Let us move forward together, working through the tangled issues one determined step at a time, and make Virginia a beacon of hope in the ongoing fight against lung cancer.
Originally Post From https://www.whsv.com/2025/11/09/new-report-shows-progress-gaps-virginias-fight-against-lung-cancer/
Read more about this topic at
The Ethical Imperative for Early Alzheimer’s Detection
Breast cancer early detection: a phased approach to …