Antibiotic Resistance: A Rising Global Concern
The growing menace of antibiotic resistance has become one of the most talked-about issues in modern medicine. With one in six bacterial infections now resistant to standard drug treatments, the World Health Organization (WHO) has raised an alert that calls for immediate attention. This opinion editorial digs into this nerve-racking phenomenon, examines its tangled issues, and considers the potential steps we can take to figure a path through an increasingly challenging healthcare landscape.
Understanding the Escalating Challenge of Superbug Infections
Recent data compiled from more than 23 million cases across 104 countries in 2023 illustrate that resistant infections have surged in about 40 percent of the pathogen-antibiotic combinations analysed since 2018. Such numbers are not just statistics—they represent lives profoundly affected by treatments that once reliably eradicated bacterial infections. When bacteria evolve and develop resistance, the hidden complexities of our treatment protocols come violently into focus, and even everyday treatments become off-putting when they fail to bring infections under control.
This alarming trend is fueled by various factors including over-prescription, misuse, and even premature termination of full antibiotic courses. When patients stop their medication too soon, believing they feel better, bacteria are given a chance to adapt, leaving behind strains that the current drugs cannot kill. Antibiotic resistance is not a limited challenge but a global problem riddled with tension that spans all regions and economic statuses.
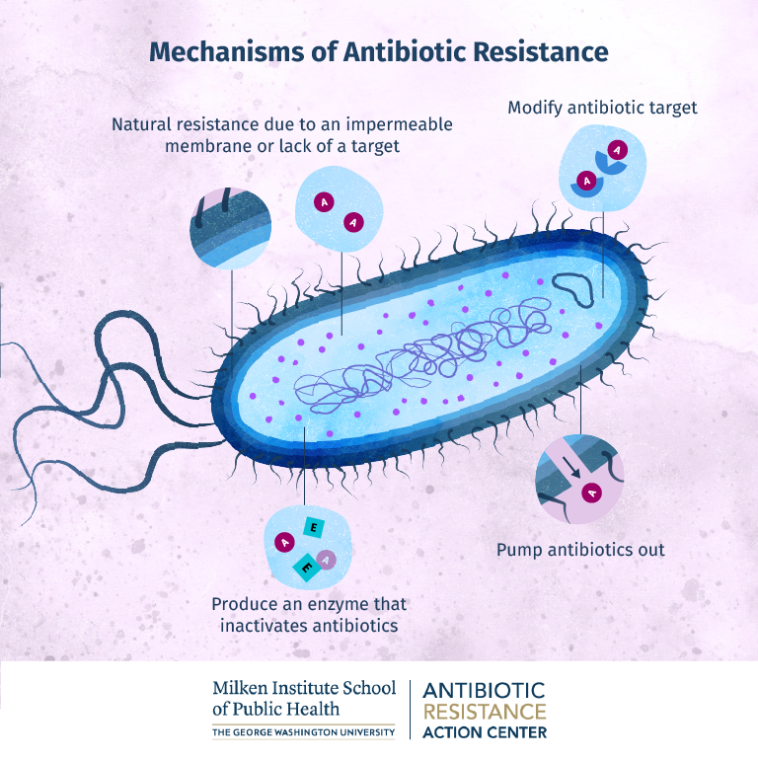
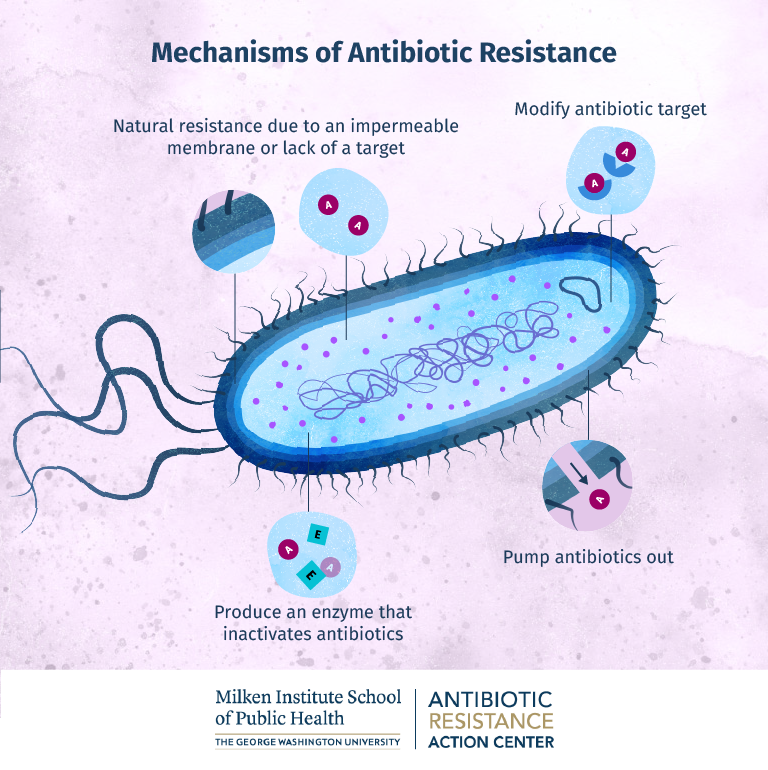
Moreover, antibiotic resistance touches upon both the small distinctions in bacterial evolution and the broad strategy of modern medicine. It is a challenge that requires us to get into the nitty-gritty of bacteria’s adaptive mechanisms while also working through strategic healthcare reforms.
Changing Landscapes in Global Antibiotic Resistance
One of the most worrying trends detailed in the WHO report is the rising resistance among Gram-negative bacteria. This group of bacteria, known for causing severe hospital infections, has shown resistance rates of over 70 percent in some parts of Africa. Such startling figures indeed underscore the nerve-racking challenges faced when handling bloodstream infections, sepsis, and other life-threatening conditions.
In regions where healthcare systems are already under pressure, antibiotic resistance compounds the problem. The intertwined issues of diagnostic capacity, antimicrobial surveillance, and access to alternative treatments form a complicated mix that healthcare professionals must untangle every day. Whether it is Klebsiella pneumoniae or Escherichia coli, the critical details concerning patterns of resistance must be closely monitored. Even the last treatment available for gonorrhoea—ceftriaxone—has begun to show signs of resistance, leading to fears that one of the world’s most common sexually transmitted infections may soon be untreatable.
This surge in resistance is not isolated to low- and middle-income countries. Data from high-income regions also show a worrying trend whereby annual deaths attributed to antimicrobial resistance are projected to increase significantly, indicating that no corner of the world is spared from these tricky parts of modern medicine.
Key Statistics on Antibiotic Resistance
| Region | Estimated Resistant Infections | Notable Observations |
|---|---|---|
| Africa | 1 in 5 bacterial infections | Rising resistance even in first-line antibiotics |
| Southeast Asia & Eastern Mediterranean | 1 in 3 bacterial infections | Heavy burden due to less robust monitoring and diagnostics |
| High-Income Nations | Projected to rise from 125,000 to 192,000 AMR-attributable deaths annually by 2050 | Even well-managed health systems face threats from resistant strains |
The table above captures some of the fine points regarding how widespread and severe the impact of antibiotic resistance is on a global scale. It is clear that action can no longer wait, as the escalating numbers signal an urgent need to steer through this public health crisis.
Implications for Healthcare Systems and Patient Outcomes
The rise in antibiotic-resistant infections does not only complicate individual patient care—it presents a broader challenge to healthcare systems worldwide. In hospitals, for instance, Gram-negative bacteria have started to play a dominant role in infections that lead to prolonged hospital stays, increased costs, and sadly, higher mortality rates. The failure of antibiotics that were once super important in managing denser infections sends shockwaves through treatment protocols and puts both patients and medical professionals on edge.
Healthcare providers now face the overwhelming task of managing treatment plans when standard interventions fall short. The exaggeration of resistance not only challenges conventional practices but also invites a domino effect where advanced therapies and alternative medicines must be digged into or even developed from scratch.
The following bullet points illustrate some of the ways in which antibiotic resistance is affecting everyday clinical practices:
- Increased Treatment Failures: Standard courses of antibiotics are proving ineffective, leading to prolonged infections.
- Longer Hospital Stays: With fewer effective treatments available, patients require extended care.
- Higher Healthcare Costs: The need for newer and more expensive drugs or treatments puts additional strain on healthcare systems.
- Risk of Epidemic Outbreaks: Resistant infections in hospital settings can lead to outbreaks, making the situation even more precarious.
These points highlight not only the tangled issues in everyday clinical decisions but also the subtle, interwoven ways in which antibiotic resistance complicates the entire healthcare ecosystem. With the current trajectory, healthcare providers must urgently get into developing more precise methods for detecting and curbing resistance.
Exploring the Causes: Misuse and Overuse of Antibiotics
At the core of the problem lies the misuse and overuse of antibiotics. When doctors prescribe antibiotics for conditions that do not warrant them—or when patients do not complete their prescribed course—the bacteria have the opportunity to adapt and grow stronger. This is one of the most intimidating aspects of modern antibiotic use. It is a problem that is, in part, driven by a lack of awareness and by the need for rapid solutions in often nerve-racking clinical situations.
There are several small but significant factors at play:
- Improper Prescriptions: Sometimes physicians, trying to act swiftly, prescribe antibiotics for ailments like viral infections which do not respond to these medications.
- Patient Non-Compliance: Patients often stop treatment as soon as symptoms improve, leaving behind bacteria that survive and evolve.
- Over-the-Counter Access: In some regions, antibiotics are available without proper prescription controls, making misuse even more common.
- Lack of Diagnostic Tools: Without access to rapid and accurate diagnostic tests, doctors may resort to a broader spectrum antibiotic approach which can contribute to resistance.
These factors form a recipe for trouble. They reflect the hidden complexities and subtle parts that add up to a global problem. Without sufficient education and stringent policies, the very measures that once protected us from infections now threaten our future ability to cure them.
Actions Required to Promote Rational Antibiotic Use
Given the multifaceted nature of antibiotic misuse, both healthcare providers and policymakers must work together to enact robust stewardship programs. Some essential strategies include:
- Educating Clinicians: Regular training sessions can help doctors stay updated on the latest guidelines, ensuring that antibiotic prescriptions are both accurate and necessary.
- Public Awareness Campaigns: Informing the public about the importance of finishing prescribed courses and the dangers of self-medication is crucial.
- Enhanced Surveillance: Governments and health organizations must invest in better monitoring systems to track resistance patterns and respond swiftly to emerging trends.
- Improved Diagnostic Tools: Investment in rapid, point-of-care diagnostic testing can reduce guesswork and help in choosing the right antibiotic from the start.
Implementing these measures can help steer through the current crisis and slow down the pace at which bacteria develop resistance. While these actions may seem like small twists in the grand scheme, they play a critical role in reining in a situation that is rapidly becoming one of our most pressing healthcare challenges.
Global Disparities: The Uneven Toll of Antimicrobial Resistance
Not all regions experience antibiotic resistance equally. While high-income countries may have access to advanced diagnostic and monitoring tools, low- and middle-income countries often bear the brunt of unchecked resistance. The WHO report brings to light that, in some parts of Southeast Asia and the Eastern Mediterranean, nearly one in three bacterial infections is resistant to typical treatments.
These disparities are rooted in several factors:
- Limited Surveillance Infrastructure: Many regions lack the sophisticated systems required for continuous monitoring of pathogen resistance.
- Poor Access to Quality Healthcare: In areas where healthcare resources are stretched thin, the opportunity for unchecked bacterial growth is significantly higher.
- Economic Constraints: The cost of newer and more effective antibiotics is often prohibitive, leading to reliance on treatments that may no longer be effective.
- Cultural Practices: In some cultures, there is a strong tradition of self-medication or reliance on unregulated over-the-counter drugs, further exacerbating the problem.
These factors create a situation where bacteria are left to evolve in an environment full of problems. It is critical that international health bodies and local governments work together to find your way through these tangled issues. Collaborative efforts should focus on improving diagnostic capacity, regulating antibiotic sales, and building stronger healthcare infrastructures.
Case Studies Highlighting Regional Challenges
Several case studies demonstrate the vast differences in managing antibiotic resistance:
- Southeast Asia: Faced with high rates of resistant infections, some countries have initiated rigorous public education campaigns and instituted strict regulations on antibiotic dispensing.
- Africa: In regions struggling with limited health resources, local health authorities are adopting innovative community-based surveillance systems to monitor resistance patterns.
- Europe and North America: Even with advanced healthcare systems, hospitals report outbreaks of Gram-negative bacteria that challenge traditional treatment protocols.
The differences observed in these case studies reveal not only the small twists that characterize microbial resistance but also emphasize the need for a tailored approach in each region. One-size-fits-all policies rarely work when the details involve various cultural, economic, and infrastructural factors.
Charting a Course Through Resistant Waters: Possible Solutions and Innovations
When we take a closer look at the current state of antibiotic resistance, two key areas demand our attention: preventing bacterial infections from becoming resistant and developing alternative treatments to safeguard public health. This dual approach is both challenging and nerve-racking, given the limited effectiveness of our current antibiotics.
Researchers and clinicians are now shifting their focus toward several innovative approaches. For instance, next-generation antibiotics and rapid point-of-care molecular tests offer promising avenues to detect and treat these infections more accurately. These solutions require a combination of scientific innovation, increased funding, and a better understanding of the biological nuances at play.
Instead of relying solely on traditional antibiotic methods, experts are now exploring other innovative treatments such as:
- Bacteriophage Therapy: Using viruses that target harmful bacteria may provide a shortcut around traditional antibiotics.
- Immunotherapy: Boosting the body’s natural defenses is another promising route. Enhancing immune responses can play a critical role in combating infections before they spiral out of control.
- Antimicrobial Peptides: Naturally occurring molecules that kill bacteria may serve as models for new drugs designed to outsmart resistant strains.
- CRISPR and Genetic Approaches: Editing the genetic material of bacteria could be a revolutionary way to eliminate the genes responsible for resistance.
Each of these alternatives involves diving in to understand the hidden complexities of bacterial adaptation. The process of developing these new therapies is filled with confusing bits and subtle parts that only time, research, and innovation can hope to overcome. Yet, they remain our best hope in ensuring that antibiotics retain their essential role in healthcare.
Building a Collaborative Future in Medical Research
A crucial element in overcoming these tangled issues is international collaboration. Researchers, governments, and pharmaceutical companies must come together to create a coordinated response. The sharing of data, findings, and resources can lead to faster development of new drugs and more effective treatment protocols. A few focal points of collaboration include:
- Global Research Networks: By synchronizing their efforts, researchers worldwide can speed up the process of testing and validating new treatments.
- Funding and Investment: Public and private sectors need to pool resources to support innovative research into next-generation antibiotics and diagnostic tests.
- Policy Frameworks: Establishing regulations that control the indiscriminate use of antibiotics can help slow the rise of resistance.
- Public-Private Partnerships: Collaborations between governments and industry can lead to breakthroughs by combining clinical insights with practical implementation strategies.
Taking these steps is crucial if we want to make headway in what has become one of the most pressing healthcare challenges of our time. By strengthening global ties, we can work through the many fine shades of bacteria’s hidden complexities to develop solutions that are as dynamic as the threats we face.
Practical Steps for Healthcare Professionals and Policymakers
The escalating trend of antibiotic resistance demands practical and immediate actions. Both healthcare professionals and policymakers are in positions where their decisions can have a profound impact on how effectively we manage this issue. Some straightforward but effective steps include:
- Enhancing Antibiotic Stewardship Programs: These programs educate healthcare providers on when and how to prescribe antibiotics, ensuring that they are used only when absolutely necessary.
- Implementing Robust Diagnostic Systems: Rapid diagnostic tests can help clinicians identify the specific pathogens causing an infection, which in turn supports more targeted and effective treatments.
- Promoting Patient Education: Public health campaigns should stress the importance of completing antibiotic courses and avoiding self-medication.
- Incentivizing Research and Development: Governments and international organizations should offer incentives for research into new antibiotics and alternative therapies.
These measures are not just band-aid solutions, but potentially transformative initiatives that can help us balance the scales in our fight against resistant infections. They represent actionable steps that can slowly unravel the complicated pieces that have led us to this critical juncture.
Strategies for Building Resilient Healthcare Systems
As we cope with the impact of resistant infections, healthcare systems need to adapt to the current trends. Some strategies to build resilience include:
- Optimizing Hospital Infection Control Protocols: Enhance sterilization methods, enforce strict hygiene practices, and invest in staff training to reduce in-hospital transmission of resistant bacteria.
- Developing Regional Centers of Excellence: Centers focused on infectious diseases can act as pulses for research, treatment, and innovative practices tailored to local needs.
- Leveraging Technology for Surveillance: Digital tools and telemedicine can help monitor outbreaks and ensure rapid communication among healthcare providers.
- Fostering Community-Based Initiatives: Local outreach programs can educate communities on antibiotic use and resistance prevention, building a network of informed citizens.
Working through these practical strategies involves tackling both the obvious and the subtle differences in healthcare infrastructures around the world. Even though each solution may address only a piece of the problem, when combined they pave the way for a more robust defense against the spread of resistant infections.
The Road Ahead: A Call for Comprehensive and Innovative Action
Antibiotic resistance is an evolving crisis that requires us to remain agile, proactive, and collaborative. The potential for runaway resistance is not confined merely to the boundaries of our hospitals, but is interwoven with public health, economic stability, and even social equity on a global scale. Working through these challenging parts and tangled issues necessitates both short-term practical measures and long-term strategic investments in medical research and healthcare infrastructure.
As we stare down the overwhelming challenge posed by resistant bacteria, we must remind ourselves that innovation and collective action are our strongest weapons. The scientific community is already hard at work on next-generation treatments and diagnostics, and the momentum in global research is growing every day. However, sustained progress will require the engagement of multiple stakeholders including healthcare professionals, policymakers, researchers, and the public.
The fight against resistant bacteria is not a battle that any one country or institution can win alone. The call for a coordinated global strategy has never been more urgent. By embracing a comprehensive approach that combines improved antibiotic stewardship, robust surveillance, and advanced medical research, we can hope to curb the spread of resistant infections and secure a safer future for everyone.
A Multifaceted Approach to Secure Future Health Outcomes
To summarize the key takeaways in our battle against antibiotic resistance:
- Prevention and Education: Emphasize educating both healthcare providers and patients about proper antibiotic use to prevent the emergence of resistant strains.
- Global Surveillance: Strengthen diagnostic tools and monitoring systems to detect resistance early and respond appropriately.
- Innovation in Treatment: Invest in and support research into novel antibiotic therapies, bacteriophage treatments, and other cutting-edge solutions.
- Policy and Regulation: Implement stringent controls on antibiotic prescriptions and sales, particularly in regions where misuse is rampant.
- International Collaboration: Foster partnerships between nations, research institutions, and global health organizations to share data and best practices.
Each of these points represents a crucial element in finding your way through this complex challenge—a challenge that is, admittedly, filled with both intimidating uncertainties and subtle differences that require continuous attention.
Conclusion: Embracing the Challenge with Informed Action and Global Unity
Antibiotic resistance stands out as a multi-layered challenge that touches every aspect of modern healthcare. From the intimidating rise in resistant infections in hospital environments to the overwhelming disparities between developed and developing regions, the issue is both pervasive and persistent. It requires us to dig into the hidden complexities of bacterial evolution, to appreciate the small twists that can make or break treatment protocols, and to commit to a future where effective drugs are not just a luxury but a global necessity.
In facing this challenge, the collaborative efforts of health professionals, scientists, policymakers, and the public are key. It is imperative to manage your way through this issue by adopting rigorous antibiotic stewardship, enhancing diagnostic capabilities, fostering innovative research, and ensuring that regulations and educational campaigns are effectively implemented.
While the path ahead is loaded with issues and may sometimes feel intimidating, the concerted efforts made today will lay the groundwork for a resilient tomorrow. The future of global health depends on our ability to work together, to make informed decisions, and to navigate the many twists and turns of antibiotic resistance with unity and determination.
By acting now, we can hope to preserve the effectiveness of antibiotics, protect vulnerable populations, and build healthcare systems that are better equipped to deal with the challenges of tomorrow. Let this serve as a call to action—a call for comprehensive, innovative, and cooperative approaches that will ultimately safeguard our collective future in the fight against resistant infections.
Originally Post From https://www.euronews.com/health/2025/10/13/one-in-six-bacterial-infections-is-now-resistant-to-standard-drugs-who-warns
Read more about this topic at
The Antibiotic Resistance Crisis: Part 1: Causes and Threats
About Antimicrobial Resistance